views
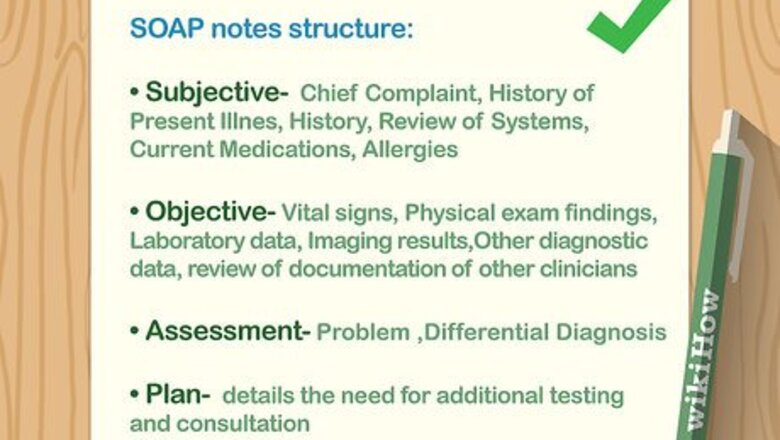
Writing the Subjective
Ask the patient about their symptoms. Talk to the patient about how they’re feeling to get an idea of the symptoms that they’re experiencing. See what their Chief Complaint (CC) is and list that at the top of your SOAP note. The CC will help other medical professionals see what the patient’s condition is so they know what to expect from the rest of the note. The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns. Some common examples may include chest pain, decreased appetite, and shortness of breath. You can also talk to a family member or spouse to get any necessary information.Tip: If the patient lists multiple symptoms, pay attention to what they describe with the most detail to get an idea of what the most concerning problem is.
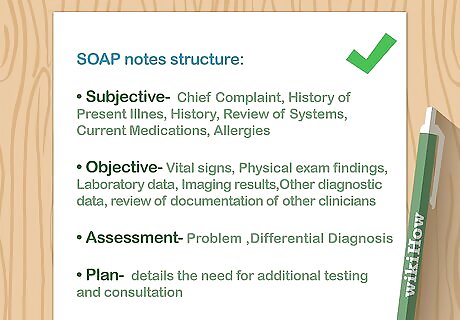
Use the acronym OLDCHARTS to get helpful information. OLDCHARTS is a mnemonic device to help you remember questions to ask the patient. Once you ask the questions for OLDCHARTS, list the patient’s answers in order to keep the SOAP note organized. The points to remember are: Onset: when did the CC start? Location: where is the CC? Duration: how long has the patient been affected by the CC? Characterization: how does the patient describe the CC? Alleviating or Aggravating factors: does anything make the CC feel better or worse? Radiation: is the CC in a single location or does it move? Temporal patterns: Does the CC occur at specific periods of time? Severity: On a scale of 1-10, with 10 being the worst, how does the CC feel?
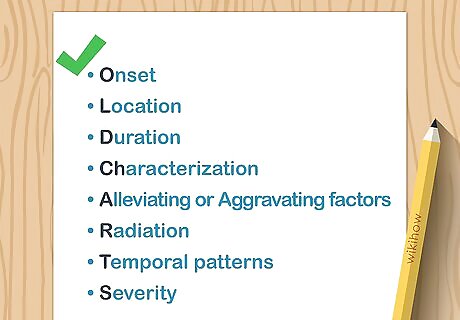
Include any medical or family history in your report. Ask the patient if they have any history with medical conditions or surgeries. If they do, try to include the year they were diagnosed and the doctor’s name who performed any surgery. See if any family members have had similar conditions or if a condition runs in the family to see if there are any genetic problems. Only write down the details that are important to your current patient. Don’t include full medical histories for relatives if they aren’t relevant.
Write down any medications the patient is already taking. Ask if the patient is taking anything, either over-the-counter or prescription, for their chief concerns. Write down the name of the medicine, the exact dosage, how they take it, and how often it’s been used. List each medication individually if there are multiple. For example, you may write: Ibuprofen 200mg orally every 6 hours for 3 days.
Taking the Objective
Record the patient’s vital signs. Check the patient’s pulse, breathing, blood pressure, and temperature and write the results down in your SOAP note. Be sure the numbers are accurate by double-checking them if they seem higher or lower than normal. Be sure to label the vitals accordingly so another professional can glance at the numbers and understand them. The Objective section of the SOAP note refers to data that you collect and measure from the patient.
Write down any information you gather from a physical exam. Assess the area that the patient is concerned about so you can write down detailed observations about it. Avoid writing the symptom that the patient is feeling; instead, look for objective signs while you’re performing the physical. Keep your notes clear and organized so they aren’t confusing to anyone else reading them. For example, instead of writing, “stomach pain,” you would write something like, “abdominal tenderness when pressure applied.”Tip: Try taking notes on a separate sheet rather than putting them directly in your SOAP note. That way, you can organize the notes more.
Include any results from special tests. Depending on the severity of the patient’s concern, you may need to run additional tests, such as X-rays or CT scans. If your patient has had specialty tests done, be sure to include any results that could affect their treatment. Include printouts of any lab data or photos from the lab tests so other medical professionals can see them first hand.
Making an Assessment
Record any changes in the patient’s problems if you’ve seen them before. If you’re not the first medical professional to see the patient, they may already have a SOAP note. Look for any changes in the patient’s concern, and be sure to list if there were positive or negative effects to prior treatment. For example, if you had previously prescribed an antibiotic, you may record how the affected area has less swelling.
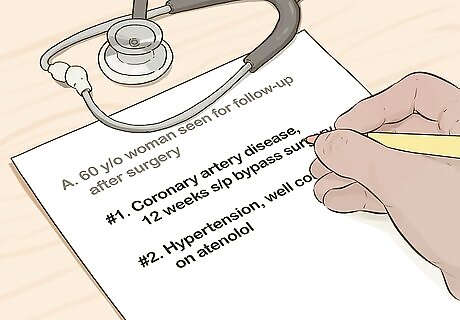
List the patient’s problems in order of importance. If the patient listed multiple concerns, start organizing them with the most severe on top and the least severe at the end. If you have trouble determining which problem is the most severe, ask them what they’re the most concerned with.

Note any diagnoses that you can make. If there is a clear diagnosis for the problem, list it immediately after the problem on your SOAP note. If there are different causes for the problem, then list them all so the most likely option is the first one. Look at the Subjective and Objective sections of your soap note to speculate what’s causing the patient’s problems. You may not know exactly what’s causing the problems, so make educated guesses based on what you’ve already found.Tip: Look for a diagnosis that covers multiple problems if you can. Be sure to list if any of the problems could interact with one another.
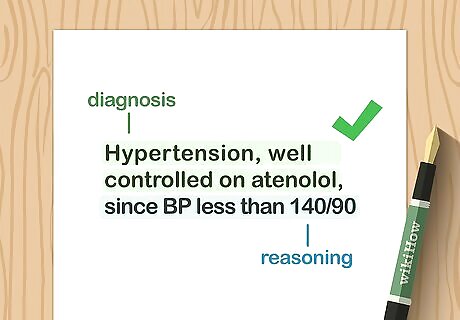
Write your reasoning for why you chose each diagnosis. Cite exact reasons from the Subjective and Objective sections of your SOAP note in your diagnoses. If you’re writing descriptions for multiple diagnoses, then be sure to include any that could conflict one another. Always leave a description so other professionals know why you made certain decisions with your treatment.
Creating a Plan
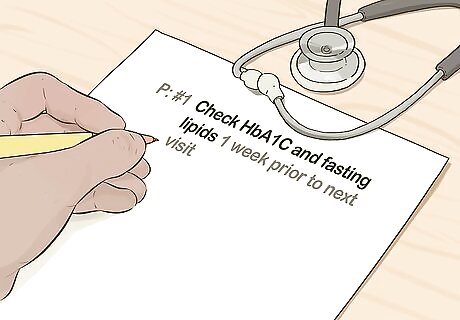
State any tests that the patient should have done next. Look at the diagnoses you wrote in the Assessment portion of the SOAP note, and determine if you need more tests to confirm them. Write down any test that fits with each diagnosis in the order of their importance. For example, you may need to perform an X-ray or CT scan to determine if there are more causes for underlying pain. List what should be done after special tests whether they come back positive or negative.

Write down any therapy or medications the patient should try. If you believe that the patient needs rehabilitation, such as physical or mental therapy, be sure to list any that can apply. If a prescription medication is more appropriate, then write the type of medication, the dosage, and how long they should take it. Sometimes, you may need to perform surgery depending on the severity of the concern.
Include any referrals to specialists if needed. If the type of care the patient needs is not your specialty, then include references for who to reach out to next. Provide names for all of the diagnoses if you still are narrowing down the cause. Let the patient know what the next steps are so they can stay informed.
Formatting Your SOAP Note
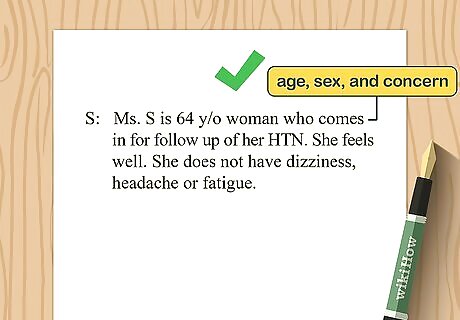
Include the patient’s age, sex, and concern at the top of the note. At the top of your note, write down the patient’s age and sex. Along with age and sex, write the patient’s concern or why they came in for treatment. This can help other medical professionals get an idea of diagnoses or treatments at a glance. For example, you may write, “45-year-old female presenting with abdominal pain,” as the first step in your SOAP note.
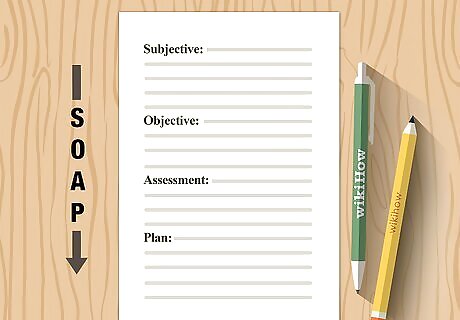
Organize the parts of your note in order. Write down all of the information that you took while working with the patient. Be sure to keep the information in order of Subjective-Objective-Assessment-Plan so other medical professionals looking through the SOAP note don’t get lost. You can choose to either use bullet points or write full sentences for notes as long as they are clear and concise. There is no required format or length for the content in your SOAP note as long as it follows the Subjective-Objective-Assessment-Plan order.Tip: Make sure any abbreviations or medical terms you use are easy to understand so they don’t cause any confusion.

Write or type the SOAP note depending on what your workplace prefers. Many systems in clinics have secure forms you can fill out on your computer so the information can be passed around quickly. However, your workplace may require you to take SOAP notes by hand. Make sure you follow the format your workplace uses closely so it stays organized.



















Comments
0 comment