
views
Reducing Risk From Pathogens and Airborne Matter

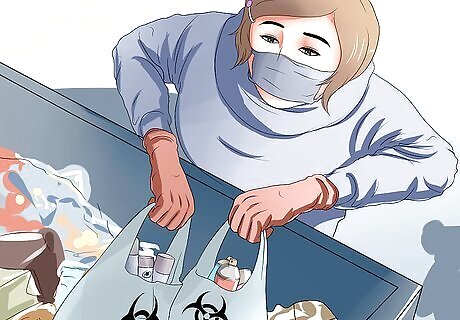
Reduce your exposure to fungal and bacterial pathogens. Pathogens are microorganisms that can cause disease. Certain species of bacteria and fungi can cause lung inflammation. Exposure to some of these pathogens is associated with occupational or environmental conditions. For example “Hot Tub Lung,” and “Farmer’s Lung” are common names for two kinds of mold-related lung inflammation. Mold can grow almost anywhere that is moist enough. According to the Environmental Protection Agency (EPA), “the key to mold control is moisture control.” To help prevent mold in your home, keep the humidity between 30-60%. If you find mold, clean the affected surface with a detergent and dry the surface completely. Prevent condensation by properly insulating areas. Avoid installing carpet in bathrooms or kitchens, where sink splashes may keep the carpet damp. Use appropriate personal protective equipment such as masks or respirators when cleaning moldy areas.
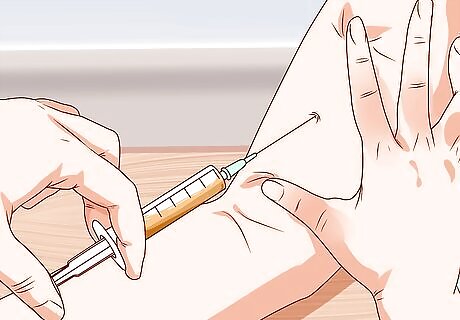
Reduce your exposure and susceptibility to viral pathogens. Influenza is a common cause of pneumonia, which is infection and inflammation of the lungs. Most cases of influenza do not lead to pneumonia, but those that do can be very serious. Influenza and pneumonia can both be prevented with vaccines. Talk to your healthcare provider to see if you are a candidate for influenza and/or pneumonia vaccinations. Avoid contact with people with influenza and/or pneumonia. If you must come into contact with people with influenza and/or pneumonia, wear appropriate protection, such as a mask, gloves, or gown.

Reduce your exposure to ambient air pollutants. Ambient air pollutants are found outdoors, and originate from natural processes, fires, and industrial operations. Six pollutants are designated as criteria air pollutants by the EPA. These include nitrogen oxides, sulfur dioxides, ozone, particulate matter, carbon monoxide, and lead. These are monitored by the EPA and are subject to a number of regulations. Particles smaller than 10 micrometers are particularly harmful, as they can get deep into the lungs. Exposure can be particularly problematic for those with pre-existing lung conditions. You can monitor the Air Quality Index in the region where you live. This information and some guidelines for exposure are available at http://www.airnow.gov/. If you are going to be in an environment where there are aerosolized particles or chemical vapors, it is important to wear proper protective equipment. Get fitted for a mask or respirator. The Occupational Health and Safety Administration (OSHA) provides guidelines about which masks or respirators are best for certain exposures.
Reduce your exposure to indoor air pollutants. Exposure to indoor air pollutants can cause headaches, fatigue, and a number of other non-specific symptoms. This sometimes causes entire buildings of workers to fall ill. Commonly encountered indoor air pollutants include combustion products, volatile organic compounds, and formaldehyde. Ventilate your home properly with clean outdoor air. Get rid of the source of the pollutants, if possible. Install a home air cleaner.
Taking Control of Your Health Care

Educate yourself about your medical conditions. In order to understand how your medical conditions may be related to lung inflammation, it is important to educate yourself. There are many helpful resources available on the internet, including Mayo Clinic, The American Lung Association, The American Heart Association, Cancer.gov, and Cancer.org. These resources have information written specifically for the layperson. Write down your diagnoses or have your healthcare provider write down your diagnoses. Ask your healthcare provider about resources to better understand your medical conditions.
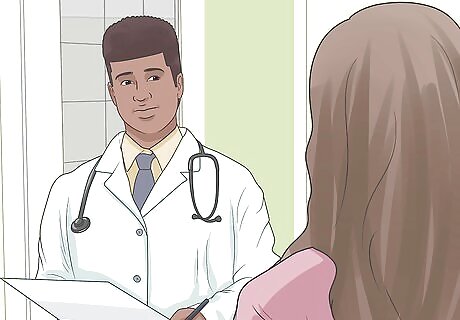
Discuss your current medications with your physician. Chemotherapy, radiation, and some medications can contribute to lung inflammation. There are other medications available that can help reduce lung inflammation, if you have been diagnosed with this condition. It is important to know what the risks from any medications or treatments are. Write down, or have your healthcare provider write down, the names of all of your medications and treatments. Ask for resources to read about the specific drugs and treatments you may be receiving.
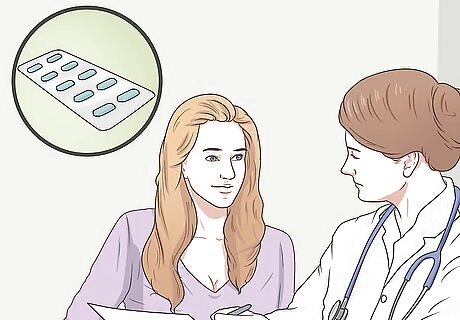
Inquire about medications available to reduce lung inflammation. There are a number of medications available that can be used to treat lung inflammation and associated conditions. The type of medication used for treatment depends on your particular diagnosis. For example, if you have pneumonia, you’ll likely be prescribed antibiotics that will help destroy pathogens causing the infection. If you have lung fibrosis, there are fewer drug options to slow the disease, but new therapies are entering the drug market. A list of drugs that can reduce lung inflammation or are used to treat related diseases are shown below. Beclomethasone dipropionate (inhaled corticosteroid used to treat COPD and asthma) Fluticasione propionate (inhaled corticosteroid used to treat COPD and asthma) Flunisolide (inhaled corticosteroid used to treat COPD and asthma) Budesonide (inhaled corticosteroid used to treat COPD and asthma) Mometasone (inhaled corticosteroid used to treat COPD and asthma) Ciclesonide (inhaled corticosteroid used to treat COPD and asthma) Methylprednisone (oral steroid used to treat COPD and asthma) Prednisolone (oral steroid used to treat COPD and asthma) Prednisone (oral steroid used to treat COPD and asthma) Hydrocortisone (oral steroid used to treat COPD and asthma) Dexamethasone (oral steroid used to treat COPD and asthma) Cromolyn sodium (inhaled nonsteroid used to treat COPD) Nedocromil sodium (inhaled nonsteroid used to treat COPD) Amoxicillin (antibiotic used to treat bacterial pneumonia) Benzylpenicillin (antibiotic used to treat bacterial pneumonia) Azithromycin (antibiotic used to treat bacterial pneumonia) Pirfenidone (drug used to slow lung scarring caused by pulmonary fibrosis) Nintedanib (drug used to slow lung scarring caused by pulmonary fibrosis) Ceftriaxone (antibiotic used to treat pneumonia and respiratory infections) Supplemental oxygen (used to ease symptoms in a wide range of lung disorders)
Making Lifestyle Changes

Quit smoking. Smoking is a major risk factor for lung inflammation, emphysema, chronic obstructive pulmonary disorder, and lung cancer. Chemicals contained in smoke are not only cancer causing, but also change how the immune system functions. Quitting smoking can be challenging, but with the correct support and planning, it is possible. There are many factors which may contribute to lung inflammation over which you have no control, but smoking is not one of them — quitting is something you can actively do to help keep your lungs healthy. Consider writing down your goals and what you don’t like about smoking. Gather a support system. Discuss your plans to quit smoking with you friends and family. Surround yourself with those who can support you. Consult a smoking cessation professional. Smoking cessation professionals can help you create a plan of attack to be successful.

Keep your immune system healthy. A major risk factor for developing pneumonia is a weakened or suppressed immune system. Those individuals who have HIV/AIDS, are organ transplant recipients, or who have been on long-term steroid therapy are at highest risk. There are some steps you can take to ensure your immune system is functioning as well as it can. Ensure you have adequate intake of Vitamin C. Vitamin C and zinc have been shown to improve the human immune system and also to improve the outcome of pneumonia and other infections. Get enough sleep. Studies have shown that individuals who do not get enough sleep are more susceptible to infections and recover more slowly after becoming ill.

Maintain a healthy weight. Though no study in humans has directly linked lung inflammation to obesity, studies in animals demonstrate a link between inflammation in the lungs and chemicals produced by fat tissue. It is thought that obesity can also increase susceptibility to infections and lung damage caused by environmental factors. Get 150-300 minutes of moderate exercise per week. Brisk walking and swimming are examples of moderate exercise. Plan to eat healthy. Eat foods high in nutrient content. Avoid processed foods and alcohol. If you need help creating a healthy eating plan, talk to a dietician. Be consistent. Sticking with your healthy eating plan, exercise, and surrounding yourself with a support group can make long-term success a reality. The Mediterranean diet can help reduce inflammation in the body, including in your lungs. Red meat and dairy can be inflammatory. Try to limit them as much as possible or switch to a plant-based diet.
Exercise your lungs, especially following surgery. The muscles surrounding your lungs can be strengthened with exercise. This can prevent infections and pneumonia, for which many people are at risk following surgery. Taking deep, even breaths can keep your lungs clear of secretions and can strengthen your lungs. In some cases, you will receive an incentive spirometer and a list of exercises. It is important to follow your healthcare provider’s recommendations with regard to exercising your lungs.


















Comments
0 comment