views
X
Trustworthy Source
US Office on Women's Health
U.S. government agency providing resources for women's health
Go to source
Some types of HPV may cause genital warts in both men and women. Other types may cause cervical cancer and other lesser known cancers in women, such as cancer of the vagina, anus, and vulva. HPV can also cause throat cancer in men and women. Recognizing HPV can be key in proper treatment or management. Some forms of HPV can be recognized on their own, while many require testing from a medical professional.
Checking For Symptoms
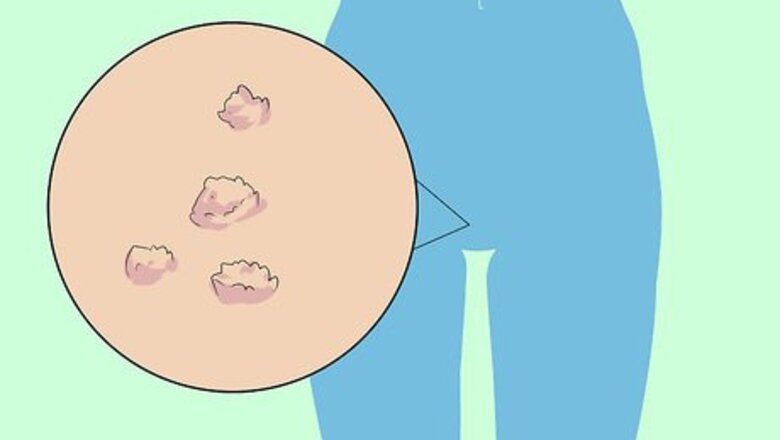
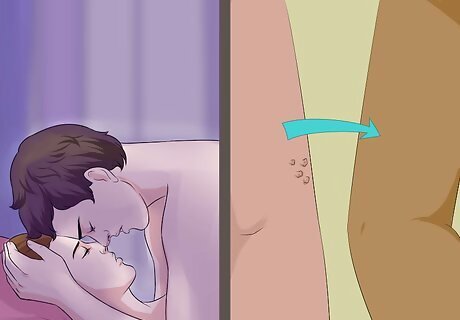
Look for warts as a symptom of low-risk HPV. The most evident symptom of a low-risk HPV infection is genital warts. These warts may appear as small raised bumps, flat lesions, or small protrusions from the skin. These warts tend to be grouped, and can show within days or weeks of infection. In women, genital warts are most often seen on the vulva and labia, but may also occur around the anus, in the vagina, or on the cervix. Low-risk HPV strains may also lead to some lesions around the cervix, but generally speaking will not lead to cancerous cell development.
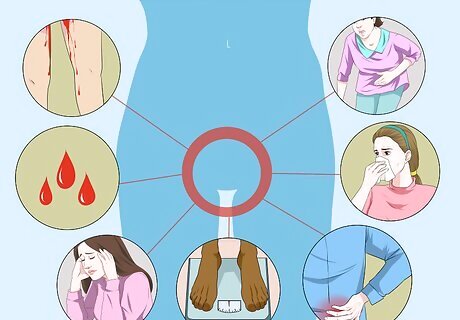
Learn about high-risk HPV detection. High-risk HPV rarely has any associated symptoms unless it has progressed to an advanced stage of cancer. This is why it is important to get an annual pelvic exam from your OB-GYN, who may be able to detect problems before they advance to a cancerous or pre-cancerous level. Symptoms of advanced-stage HPV that may be causing cervical cancer include: Irregular bleeding or spotting between periods or after sexual intercourse. Irregular menstrual cycles. Fatigue. Weight loss or loss of appetite. Back, leg, or pelvic pain. A single swollen leg. Vaginal discomfort. Odorous discharge from the vagina.
Screen for other cancers. High-risk HPV most commonly causes cervical cancer, but it has also been linked to cancer of the vulva, anus, and throat. These cancers can be detected early if you get regular medical examinations, which is why it is important to get regular screenings. On exposed areas, such as the vulva or around the anus, swipe a flat palm over the area to check for lumps that may indicate genital warts. If you believe you have been exposed to HPV at any point, alert both your OB-GYN and your general practitioner, and ask them to screen you for any potential cancers associated with HPV.
Distinguishing HPV
Get tested to determine the type of HPV. There are upwards of 100 different viruses that are considered a form of HPV. Of those 100+ strains, around 40 of them are sexually transmitted, while around 60 of them cause warts on areas such as the hands and feet. Non-sexually transmitted HPV usually enters your body through skin-to-skin contact, entering through cuts or abrasions on the skin, and will manifest as warts around the area of infection Sexually transmitted HPV enters the body through direct genital contact, or from skin-to-genital contact. HPV infections around the mouth or in the upper respiratory system may also occur from oral sex. These may manifest as warts, or may have no symptoms. Only a test from your doctor can properly diagnose sexually-transmitted HPV.
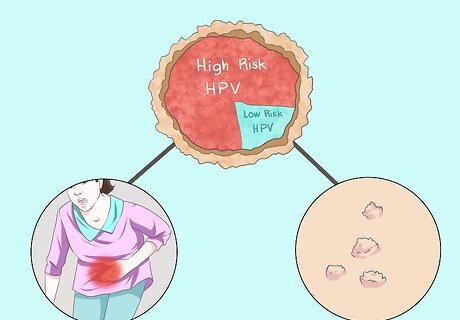
Consider whether you have sexually transmitted HPV. Sexually transmitted strains of HPV are generally broken down into two broad categories: high risk and low risk HPV. About 40 types of HPV are transmitted by direct contact with a mucus membrane, such as those around the genital area. These types are the most likely to be spread through sexual contact. High-risk HPV viruses are those that are sexually transmitted and are at a higher risk for developing into a serious health risk, such as cancer. High-risk HPV strains include HPV 16, 18, 31, 33, 45, 52, 58, and a couple other strains. The strains responsible for most cervical cancer development are 16 and 18, which are screened for most commonly since they cause about 70% of cervical cancers. Medical testing is necessary to see if you have high-risk HPV. Low-risk HPV strains include HPV 6, 11, 40, 42, 43, 44, 53, 54, 61, 72, 73, and 81. HPV 6 and 11 are the most common forms of low-risk HPV, and are the HPV strains most commonly associated with genital warts. Rarely do low-risk strains lead to cancer, so they are not part of routine screening.
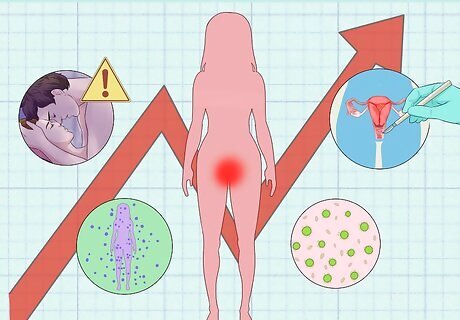
Evaluate your risks. Certain factor can increase a woman’s chance of contracting HPV. Those who have had multiple sexual partners, a weakened immune system from HIV, immune disorders, or cancer treatment, and those who engage in unprotected sex may all be at a higher risk for sexually-transmitted HPV. Aligning with a risk factor does not mean that a woman has or does not have HPV. It is simply an indicator that she is more likely to be exposed.
Seeking Medical Advice
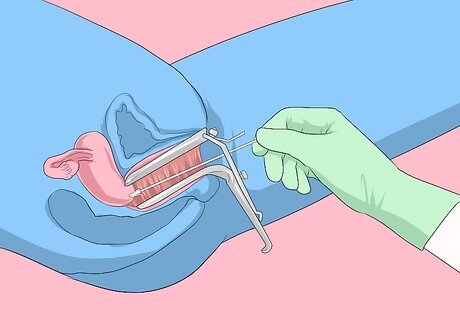
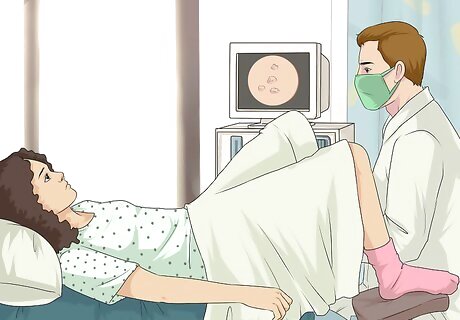
Get a Pap test. Pap tests are the primary method for a doctor to check for cervical cancer or precancerous changes to the cervix. If a Pap test comes back irregular, the doctor may opt to perform an HPV DNA test to see if the Pap sample tests positive for HPV. However, some doctors also perform both tests together. Pap tests are recommended every three years for women under the age of 65 whose previous Paps have come back normal. If you receive an irregular Pap result, your doctor will advise you on a good testing schedule.
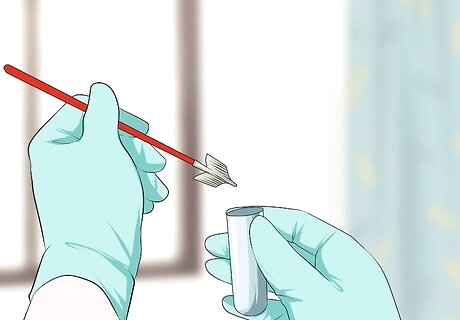
Ask for an HPV test along with your pap test. HPV tests are may not be given as part of a routine exam for women, but many doctors perform both tests together. You can request an HPV test along with your pap test if you believe you have reason to worry. Samples for an HPV test are collected the same way as those for a Pap test, by swabbing the cervix. HPV tests are generally only recommended for women age 30 or over, and thus a doctor may not recommend one for younger patients. HPV is common in young women, and most strains are cleared up by a healthy immune system before any symptoms or complications can occur. Subsequently, your doctor may recommend another screening method, such as a Pap test, to see if there is any need for concern or further testing. At this point, HPV tests have only been effectively developed for women. Thus, a woman cannot ask a male partner to get screened for HPV in order to assess their risk.

Get any warts screened. If you notice any warts, lesions, or lumps around your genital area, contact your doctor immediately. Set up an appointment to have the doctor look at any warts or suspicious symptoms as soon as possible. Genital warts often go away on their own, and depending upon your specific symptoms your doctor may recommend careful monitoring and no further treatment. If your doctor does recommend treatment, they may opt for topical treatments or freezing the warts. Ask your doctor if your treatment can be applied at home, or if it must be done by a medical professional. If you receive treatment for genital warts, ask your doctor, “What should I do to prevent infection in this area and minimize risk of future warts?”

Talk to your doctor at your annual checkup. Be sure to talk with your doctor about any concerns you have about HPV. Part of a well woman exam is also an examination of the vulva, vagina, and anal area. If you are concerned that you are at risk for HPV infections, then let your doctor know so that these areas can be examined too.
Preventing HPV Infection
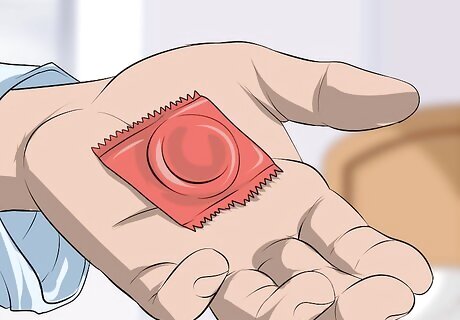
Use a condom. When used correctly, condoms are 97% effective against most sexually transmitted infections. Use a condom any time you have vaginal or anal intercourse, and opt for protection such as a dental dam during oral sex. To properly put on a condom: Inspect the wrapper for any cuts, holes, or punctures, and look for the expiration date. Do not use an expired condom or one that appears to be damaged. Carefully open the wrapper to ensure that the latex of the condom does not tear. Remove the condom and pinch the tip before rolling down the shaft of the penis. While still pinching the tip of the condom with one hand, line the condom up with the head of the penis and use your other other hand to roll the condom down the shaft of the penis to its base. Dispose of a used condom by tying off the open end and placing in a waste receptacle.

Get vaccinated. Vaccines that guard against certain high-risk strains of HPV are now readily available to women and boys. It is recommended that girls get the vaccine between ages 11 and 12, but it may be administered at any point between ages 9 and 26. Boys can get the vaccine at ages 11 or 12, or up to age 21. The vaccine is ideally administered before a girl or woman becomes sexually active, but may still benefit sexually active young women. HPV vaccines are generally given as a course of three shots over six months.

Discuss sexual history. Whenever you begin having sex with a new partner, have an open and honest discussion about your sexual history with your partner. Talk about what types of testing and screening you’ve had recently, and how many sexual encounters you have had since your last test or examination. Take the time to discuss your sexual history before you begin having sex with a new partner. Do not be afraid to ask them specific questions such as, “Have you noticed any symptoms that may be related to HPV such as warts?” and, “How many sexual partners have you had?” Do respect a person’s decision to not share information with you if they do not want to, but also understand that you are under no obligation to have sex with anyone and may choose to not engage in intercourse if you cannot get the information you need to feel comfortable consenting.

















Comments
0 comment