
views
Tapering off Zoloft
Talk to your doctor. Discuss your side effects or other reasons for wanting to stop taking Zoloft with your doctor. This will help your doctor make an informed decision and decide if the time is right for you to stop taking Zoloft. If you have been on the medication for less than eight weeks, your doctor will likely suggest you give the medication the full eight weeks to take effect. If you feel like stopping Zoloft because it hasn't been effective, you may want to ask your doctor if increasing your dosage might have positive results.

Discontinue Zoloft slowly. Antidepressants need to be slowly discontinued with gradual decrease in doses to avoid discontinuation symptoms. This is called tapering. Tapering can take weeks to months depending on the antidepressant, how long you have taken it, your dose, and your symptoms. If you stop right away—go “cold turkey”—your body does not have enough time to adjust, and you may experience worse discontinuation symptoms. Symptoms may include: Abdominal issues such as nausea, vomiting, diarrhea, or cramps Sleep issues such as insomnia or nightmares Balance issues such as dizziness or lightheadedness Sensory or movement issues such as numbness, tingling, tremors, and lack of coordination Feelings of irritability, agitation, or anxiety

Taper based on your doctor’s schedule. The length of time it takes to completely stop taking Zoloft may depend on how long you were on the medication and the dose you were prescribed. Your doctor will determine the best schedule for you to taper off Zoloft while minimizing the potential for discontinuation symptoms. One suggested way is decreasing the dose by 25mg per dose reduction, giving at least two weeks in between each dose reduction. Keep track of your tapering schedule by writing down the dates and the dosage changes. Expect to taper off the medication over several weeks. If you were on Zoloft for a long time, then you will likely taper off of it over four to six weeks. If you start to experience intolerable withdrawal symptoms, then your doctor may decide to taper the dosage at a slower rate.
Document any effects you experience. Even if you are tapering Zoloft, it is still possible to experience discontinuation symptoms. You may also be at risk of experiencing a relapse with regard to your depression or disorder. Keep track and talk to your doctor if you develop any of these symptoms. Discontinuation symptoms have a quick onset, slowly get better over 1-2 weeks, and include more physical complaints. In order to differentiate between relapse and discontinuation symptoms, look at when the symptoms start, how long they last, and the type of symptoms. Relapse symptoms gradually develop after 2-3 weeks and get worse over 2-4 weeks. Contact your doctor if any symptoms last more than 1 month.

Keep your doctor informed. Your doctor will monitor you for at least a few months after discontinuation. Inform him or her about any relapse symptoms or concerns you may have. You may want to follow-up with your doctor more closely during this time period.

Take any new medications according to your doctor’s prescription. If you are discontinuing Zoloft because of side effects or if Zoloft is not controlling your depression, your doctor may prescribe a different antidepressant. The choice of medication depends on many aspects such as patient preference, prior response, effectiveness, safety and tolerability, cost, side effects, and drug interactions. If you experienced side effects or inadequate control of your depression, you doctor may recommend: A different selective serotonin reuptake inhibitor (SSRI), including Prozac (fluoxetine), Paxil (paroxetine), Celexa (citalopram), or Lexapro (escitalopram) Serotonin norepinephrine reuptake inhibitors (SNRIs), such as Effexor (venlafaxine) Tricyclic Antidepressants (TCA), such as Elavil (amitriptyline). Monoamine oxidase inhibitors (MAOIs) can also be used after waiting at least five weeks after discontinuation of Zoloft.
Including Lifestyle Changes and Alternative Therapies
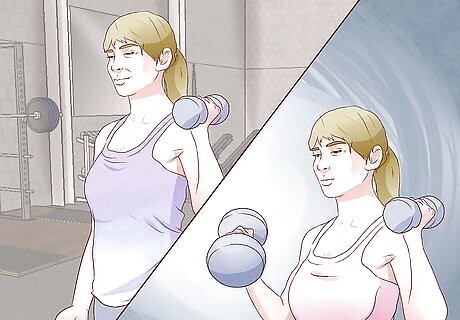
Try to exercise regularly. Studies show that regular exercise can help produce endorphins and increase neurotransmitters that may help with symptoms of depression and anxiety.Try to exercise for approximately thirty minutes each day.
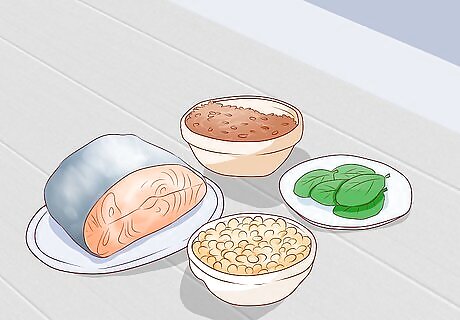
Change your diet. A healthy diet can help you overall. In particular, omega-3 fatty acids have been shown to help as an adjunctive therapy for depression. Omega-3- fatty acids are contained in foods such as kale, spinach, soybean or canola oil, flaxseeds, walnuts, and fatty fish such as salmon. They are also available over the counter, usually as fish oil gelatin capsules. Studies that showed benefit of omega-3 fatty acids in mood disorders included doses between 1–9 grams (0.035–0.32 oz). However, more evidence supports the lower doses in that range.

Follow a consistent sleep schedule. Sleep is often disturbed by depression. It is important to follow good sleep hygiene to ensure you are getting proper rest. Good sleep hygiene includes: Going to bed and getting up the same time each day Avoiding stimulation before sleeping, such as exercise, watching TV, or doing computer work Avoiding alcohol and caffeine before bed Associating your bed with sleep as opposed to reading or doing other work

Get some sun. There is not a consensus on how much exposure you need to help symptoms of depression. However, researchers agree some types of depression, such as seasonal affective disorder, may benefit from getting more exposure to sunlight. Research also suggests sunlight can affect your levels of serotonin. Sunlight may also decrease the risk for disorientation and depression in older patients with Alzheimer's. Generally, there isn’t a maximum amount of exposure for sunlight. Make sure you do wear sunscreen if you are going to be in the sun longer than 15 minutes.
Have a good support system. Throughout the process, stay in touch with your doctor and let your doctor know about your status, feelings, or symptoms. Keep a relative or close friend involved as well. They may be able to provide emotional support or recognize signs of relapse. Having a good support system is very important. Try not to turn down invitations to activities, and try and get out more often.

Consider psychotherapy. An analysis of different studies found that people who undergo psychotherapy while discontinuing an antidepressant are less likely to have a relapse. Psychotherapy is a way to help people with mental disorders by teaching them ways to deal with unhealthy thoughts and behaviors. It gives people tools and strategies to manage their stress, anxieties, thoughts, and behaviors. There are different types of psychotherapy. Treatment plans depend on the individual, the disorder, severity of disorder, and numerous other factors such as if you are on medications. Cognitive behavioral therapy’s (CBT) goal is help a person think more positively and influence behavior. It focuses on current problems and solutions to those problems. A therapist helps the person identify unhelpful thinking and change inaccurate beliefs, thus aiding a change in behavior. CBT is particularly effective for depression. Other therapies—such as interpersonal therapy, which focuses on improving communication patterns; family-focused therapy, which helps by resolving family conflicts that may be influencing the patient’s illness; or psychodynamic therapy, which focuses on helping people gain self-awareness—are also available options.

Consider acupuncture. Some studies have shown benefits of acupuncture for depression. Although it is not part of guideline recommendations, acupuncture can be useful for some. Acupuncture is a technique in which thin needles are inserted through the skin to stimulate specific points on the body and relieve symptoms of diseases. If needles are sterilized properly there is little concern for risks.

Consider meditation. A Johns Hopkins analysis of previous studies suggests that thirty minutes of daily meditation may improve symptoms of depression and anxiety. Practical ways you can practice meditation are repeating a mantra, prayer, taking time to focus on breathing, or reflecting on what you have read. Aspects of medication include: Focus - Focusing on a specific object, image, or breathing can free your mind of worry and stress. Relaxed breathing - Slow, deep, even paced breathing increases oxygen and helps you breathe more efficiently. Quiet setting - This is an important aspect to meditation, especially for beginners, so that you have fewer distractions.



















Comments
0 comment