
views
- Look for tell-tale signs of a blood clot in your leg like abnormal swelling, discoloration, or skin that’s warm to the touch.
- See a doctor if you suspect you have a blood clot, as DVT could be the start of more threatening conditions.
- If you experience shortness of breath or pain while breathing, go to the emergency room. This could mean the clot has traveled to your lungs, which is life-threatening..
Signs of a Blood Clot in Your Leg
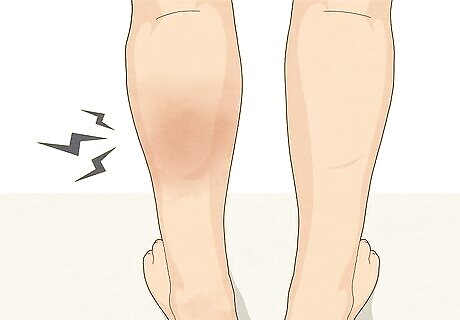
Watch for swelling in your leg. A blood clot can block the blood flow in your leg, causing it to swell and ache. Gently feel your affected leg and then feel your unaffected leg. Is one bigger than the other? The swelling may be slight and you may only notice it when putting on clothing like pants, workout gear, or high boots. Sometimes, swelling alone can be the only presenting symptom of DVT.

Notice if your leg hurts or is tender. Many people with DVT experience aches, cramps, and Charley horses in their affected legs. Keep a log of when you notice different sensations in your leg. For instance, write down if the cramping starts during or after exercise or suddenly happens when you’re resting on the couch. This way, your doctor can rule out any other possible medical conditions or injuries. Pain typically occurs when walking or standing but could happen at any moment without cause, so it’s important to document when it happens. In most cases, the pain will start in the calf and radiate from there.

Feel if your leg is warm around the swollen or sore area. Sometimes, a leg will feel warm to the touch if you have a blood clot. Place a hand on either side of your leg. Does one side feel warmer than the other? Then, place your hands on your other leg. Is there a significant difference between the two? If so, you may have a blood clot. Be aware that the increased warmth may only be in the swollen or painful area of the leg. Feel your entire leg to easily detect a section that is warm versus one without a temperature difference.

Look for skin discoloration around the swollen or painful area. Many patients with DVT notice red or purpling skin around the area of their leg that hurts. Notice if you have abnormal reddish or bluish skin patches on your leg. These may look like bruises, but they’re most likely a sign that blood isn’t circulating properly under the surface. Bruises change color over time, while discoloration from a blood clot won’t.
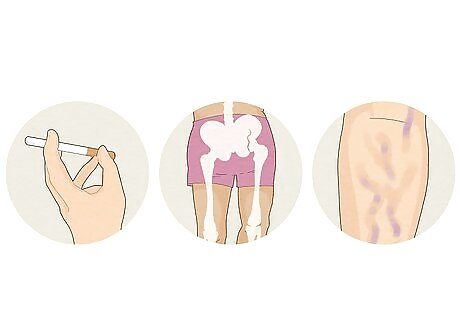
Recognize your risk factors for developing a blood clot. Almost anyone can develop a blood clot in their leg; however, some individuals may have a higher risk than others due to their age, medical history, and lifestyle. You’re more susceptible to blood clots if you: Are 65 or older Had a recent surgery Take birth control or other hormones Smoke Have broken a hip, pelvis, or leg Have or have had cancer Are overweight Are on bed rest Have had a stroke Are paralyzed Have a portacath Have varicose or bad veins Have a family member has had a blood clot before Have had a blood clot before Have taken a long trip on a car, plane, bus, or train

Go to the ER ASAP for pulmonary embolism symptoms like sharp chest pain. If you have a blood clot, you’re susceptible to pulmonary embolism (PE), which is caused by a piece of the blood clot breaking off and entering your lungs. Check into the emergency room right away if you have one or more of these symptoms: Sudden shortness of breath Sharp or stabbing pain when breathing that worsens with deep breaths Rapid heart rate Sudden bouts of coughing, which may contain blood or mucus Fainting or feeling dizzy or lightheaded
Getting a Medical Diagnosis
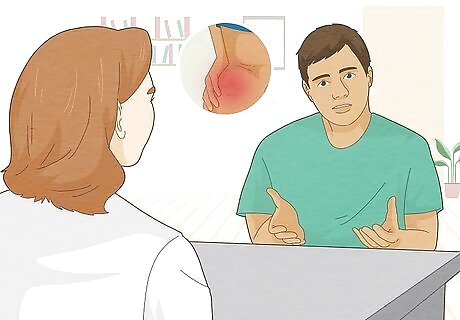
Tell your doctor about your symptoms immediately. The only definitive way to know if you have a blood clot in your leg is to get a medical diagnosis. If you experience any symptoms, call your doctor or go to the emergency room as soon as possible. Blood clots can be extremely dangerous if left untreated, leading to further complications like a pulmonary embolism. Answer any questions your doctor may have about your symptoms, such as when they started or what makes them better or worse. Make sure to tell your doctor about medications you’re taking, if you’ve been treated for cancer, or if you’ve had any recent surgeries or injuries.

Undergo a physical exam to check for signs of a blood clot. Before your doctor orders more involved tests, they’ll perform a physical exam to check for signs of DVT. The doctor will most likely touch and feel your legs while asking questions about your pain. Along with this, they may check your blood pressure and listen to your heart and lungs. Don’t be afraid to tell your doctor if something they do or touch hurts—your pain can help diagnose you properly.

Partake in diagnostic testing to get a detailed diagnosis. Your doctor may order additional tests to determine whether or not you have DVT. Further testing isn’t something to worry about—it’ll help your doctor find and treat your symptoms effectively. The most common diagnostic tests for DVT are: Ultrasound: This is the most common test for DVT and involves taking pictures of the leg veins and arteries. D-dimer test: This blood test measures a substance in your blood released when a clot breaks up. High levels can indicate a deep vein blood clot. Spiral CT of chest or ventilation/perfusion (VQ): These scans are used to rule out a pulmonary embolism. Venography: This test is similar to an ultrasound but gives a doctor a clearer image of the arteries and shows the blood flow direction. The procedure requires injecting a dye and x-raying the vein. Magnetic resonance imaging (MRI) or computer tomography (CT): These scans take pictures of the organs and are generally used to diagnose PE.
Treating & Preventing Blood Clots in Your Legs

Wear compression stockings to prevent swelling. One of the easiest things you can do to prevent blood clots at home is to wear compression stockings. These tall and tight socks squeeze your legs and improve blood flow, helping prevent future clots. Doctors will often prescribe this at-home treatment along with medication or lifestyle changes to keep blood clots from returning. Have compression socks fitted by your doctor or medical supply professional before buying them to ensure you get the right amount of compression. Your doctor may advise you to wear stockings for 2 to 3 years if you’re at higher risk for blood clots.

Start a healthy diet and exercise regime to clear blood clots naturally. Another great way to reduce your risk of getting a blood clot is to make specific lifestyle changes. Talk to your doctor about what you can improve or change in your life to lessen your risk. For instance, they may suggest you: Eat less salt Exercise daily Wear loose-fitting clothing Avoid putting pillows under your legs Change positions often, especially on long trips Avoid sitting or standing for more than an hour at a time
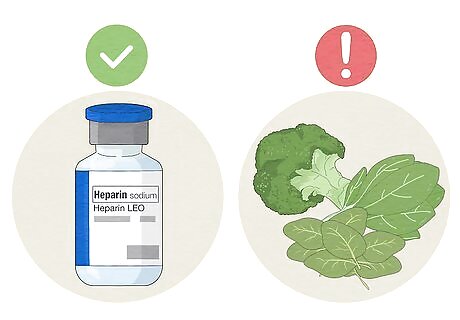
Take anticoagulants to reduce your chances of getting another clot. If your doctor diagnoses you with DVT, they may give you an anticoagulant or blood thinning medication to prevent future complications. These medications can be taken in the form of a pill, injection, or IV, depending on the severity of your condition. Follow your doctor’s instructions for taking the medication, as taking too much or too little could have serious side effects. Ask your doctor any questions you may have about taking blood thinners, and make sure to discuss potential side effects you should be aware of. Common blood thinners include Heparin, Warfarin, Enoxaparin (Lovenox), Dalteparin (Fragmin), and Fondaparinux (Arixtra). Know that foods rich in vitamin K, like spinach, kale, and Brussels sprouts, can interfere with blood thinning medication. Patients with acute DVT often require hospitalization for anticoagulation therapy to treat and minimize the size of the blood clot.
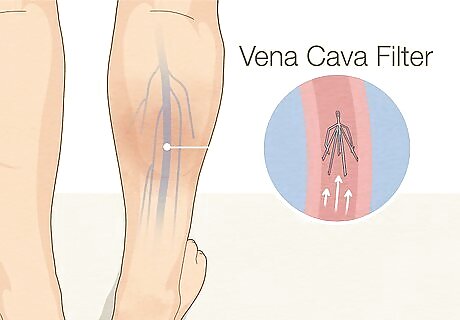
Have a vena cava filter medically inserted to prevent blood clots. If you can’t take blood thinning medication, your doctor may suggest surgically placing a filter in your vena cava (the large vein in your abdomen). This filter helps prevent blood clots that have broken loose from your leg from entering your lungs. This medical treatment is beneficial if you’re at risk for PE.
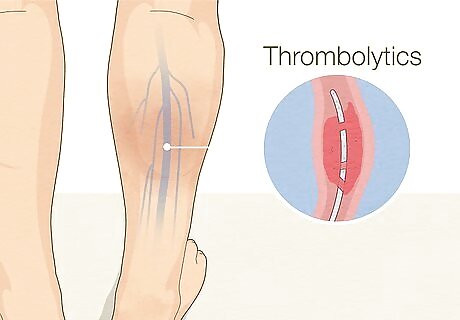
Dissolve stubborn clots with thrombolytics. Severe cases of DVT may require medications called thrombolytics or clot busters. These medications dissolve clots faster than your body naturally could, helping minimize the risk of complications and infections. Understand that thrombolytics can cause excessive bleeding and are only prescribed in severe or life-threatening cases. Because of the severity, thrombolytics are only given in a hospital’s intensive care unit. A doctor will administer the drugs through an IV or catheter placed directly into the clot.
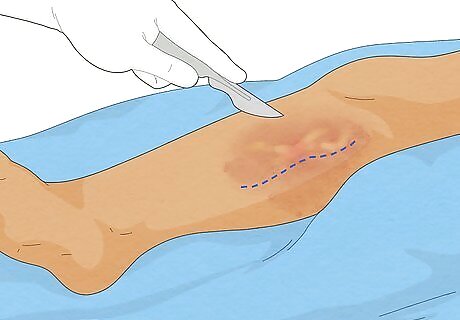
Have surgery if your doctor recommends it. Thrombectomy is a type of surgery used to remove the clot from the artery or vein directly. This procedure is used in rare cases, such as if the clot is especially severe, getting worse, or not responding to medication. Every surgery comes with risks, and there’s no 100% guarantee that a thrombectomy will prevent the blood clot from forming again or developing into a pulmonary embolism.


















Comments
0 comment