views
X
Trustworthy Source
PubMed Central
Journal archive from the U.S. National Institutes of Health
Go to source
When the lymphatic system isn’t working correctly, some of your body’s waste goes unfiltered and builds up in an arm or leg which triggers swelling. While recovering from trauma, infection, surgery or fighting cancer is hard enough, take solace in the fact that lymphedema is extremely manageable and there are plenty of ways to relieve your symptoms.
Recognizing Symptoms of Lymphedema
Check for swelling in one area of your body. While lymphedema are most common in your arms and legs, they can also occur in your trunk, abdomen, head, neck, or genital area. At first, you'll likely notice that you can press the swollen area and the mark will remain for some time. However, the swollen area may grow in size and get harder as tissue builds up. Consult your doctor if you see any swelling on your body that you suspect may be a lymphedema. Your skin may look puffy or could look like it has a lump under it.
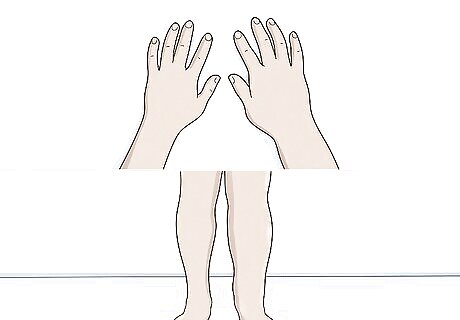
Compare your arms and legs to see if they’re the same size. Set both of your arms in front of you and compare the thickness of your wrists, forearms, and fingers. Then, stretch both feet out in front of you and compare your shins, toes, and thighs. If one of your limbs is noticeably thicker than the opposite arm or leg, you may have lymphedema.Tip: If you’re receiving cancer treatment or you just had surgery and one of your limbs is visibly swelling, you almost certainly have lymphedema. Call your doctor immediately and keep the limb elevated until you can get in to see them. You can measure each limb with a cloth measuring tape if you’d like, but don’t worry too much about minor differences you find. Your limbs may be naturally a little different, or you may have a sore muscle causing minor discrepancies. Lymphedema is typically a uniform difference over a larger portion of your limb.
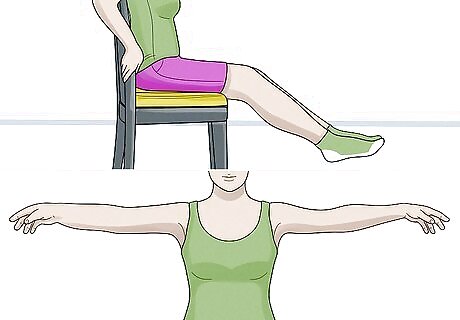
Lift your arms and legs at the same time to see if one feels tight or heavy. Sit down and stick your feet up in front of you. Move your legs back and forth. Then, try raising them separately while standing and note the feeling with each leg. Do a similar exercise with your arms by lifting them at your sides and over your head. If your range of motion is impaired or one of your limbs feels heavier than the other, you may have lymphedema. The heaviness may be kind of subtle and you likely won’t notice it unless you raise your limbs at the same time. Take any jewelry off when you lift your arms and keep your shoes off when you raise your feet. You don’t want any false positives from a water-logged boot or heavy watch!

Feel the skin on all of your limbs to spot inconsistencies or pain. Lymphedema causes fluids to build up in one limb, which typically changes the texture of the skin. Feel every portion of each arm and leg to see if you find any strange-feeling skin. Occasionally, the affected skin will hurt when you touch it. Gently poke any skin you find that doesn’t match the rest of your body to see if it hurts. These symptoms are not universal and you can still have lymphedema if your skin is uniform and you aren’t in pain. However, the odds are much higher you have lymphedema if the skin is affected.
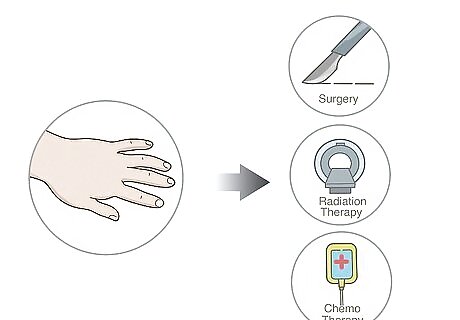
Assess the timeline of your symptoms to see if they were triggered by treatment. The vast majority of lymphedema cases are triggered by cancer treatment, radiation, or surgery. This is known as secondary lymphedema and it makes up roughly 90-98% of all lymphedema cases. If you’re fighting cancer and you’re in treatment or you’ve had surgery in the past 1-12 weeks, this likely triggered your symptoms. When the condition isn’t caused by anything, it’s known as primary lymphedema. This form is almost always caused by hereditary or genetic factors. It’s hard enough to fight cancer to begin with so getting lymphedema can be especially frustrating. Try not to get too down about it—this is an extremely common complication and there are plenty of ways to manage the symptoms.
Taking a Diagnostic Test

Talk to your primary care doctor about confirming the condition. Schedule a doctor’s appointment If you recognize one or more of the common symptoms. Let them examine your symptoms and tell them about what you’re experiencing with your limbs. The doctor may be able to confirm the condition in the examination room, although they’ll likely order at least 1 diagnostic test to confirm their suspicions.Tip: Lymphedema is rarely life-threatening unless it goes untreated for an extended period of time. Try not to worry too much; it is an extremely treatable and manageable condition.

Let the doctor check for a Stemmer’s sign on your second toe or finger. Your doctor will pinch the skin on the top of your index finger or long toe. They are looking for a Stemmer’s sign, which is a thickened fold of built-up skin that develops under the second finger or toe. If they find this fold, they’ll confirm the diagnosis on the spot. The good news is that there are no false positives with the Stemmer’s sign and you’ll be able to skip any other diagnostic tests you would have needed otherwise. However, not having this skin fold does not necessarily mean that you don’t have the condition. You can try checking for this at home, but your doctor will have a better idea of what they’re looking for.
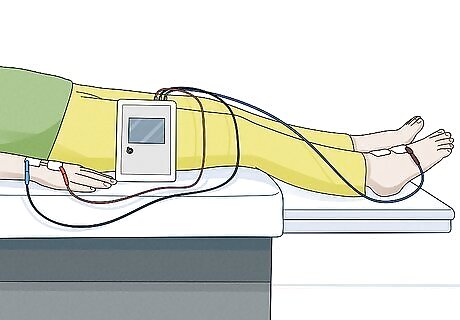
Get an l-dex assessment to see if the limb is filled with fluid. Your doctor may order an l-dex assessment to reach a diagnosis. This is a noninvasive test where electrical signals are sent down your limbs and measured to see if there are any discrepancies or blockages. Show up at the department or lab you’re referred to and let the nurse or specialist complete the test. You’ll find out immediately if the signals match or not. If the signals do match, you do not have lymphedema and any other symptoms you’re experiencing are the result of some other issue. If the electrical signals do not match, it means there is a buildup of fluid in your limb interfering with the signal. This is an accurate way to determine if you have lymphedema. This sounds like a scary procedure, but it’s actually painless. You just lie still and the nurse or specialist puts a patch connected to a wire on each limb.
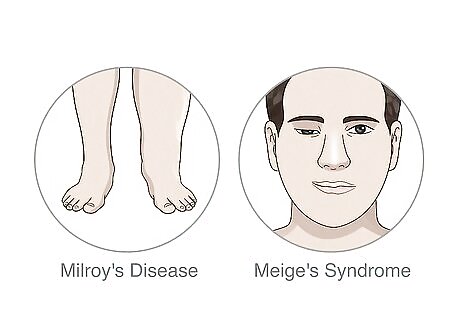
Ask about Milroy’s or Meige’s syndrome if cancer and surgery are not factors. If the diagnosis is confirmed but you aren’t in treatment for cancer or recovering from surgery, ask your doctor to test for Milroy’s disease and Meige’s syndrome. Lymphedema is a symptom of both of these rare diseases, but they’re treated differently than an isolated case of lymphedema. Common symptoms of Milroy’s disease include cellulitis, enlarged testicles in men, and angled toenails. This is an incurable hereditary disease, but it’s extremely treatable with medication. Meige’s syndrome is often associated with involuntary eyelid movements and twitches in the face and jaw. This is a rare neurological disorder and the cause is unknown. Unfortunately, it’s incurable, but you can manage the symptoms with medication. Late-onset lymphedema (also known as hereditary lymphedema) is a third possibility, but it’s extremely rare. This is a genetic lymphatic disorder that is fairly difficult to treat. You may need periodic surgery to combat the symptoms.
Coping with the Condition

Talk to your doctor to weigh your treatment options. If the lymphedema is developed, you cannot cure it. Luckily, there are plenty of successful treatment options available. Talk to your doctor about treating the symptoms. In most cases, compression and periodic massages can help ease the swelling and reduce fluid buildup.
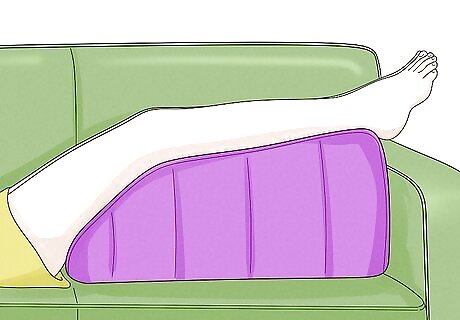
Elevate the limb to reverse stage 1 lymphedema by draining the fluids. If your doctor confirms stage 1 lymphedema, which is the mildest form of the condition, you can actually reverse the symptoms. To do this, lie down and prop your leg up or sit down and rest your arm on an elevated surface. Take breaks when the limb gets uncomfortable or tingly and repeat this process as long as you reasonably can. Over time, your limb will drain and the damage may be reversed.Tip: You can only do this if you have stage 1 lymphedema, also known as spontaneously reversible lymphedema. This type of lymphedema is usually caused by gravity, not lymphatic damage. Elevating your limb will typically reduce pain as well. Prop your leg or arm up if you feel a surge of pain coming on even if you don’t have stage 1 lymphedema.
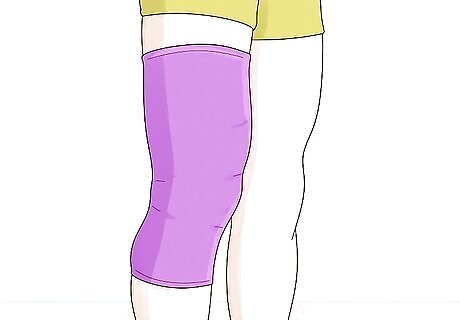
Wrap the swollen limb in a compression sleeve to alleviate pain. Get a compression sleeve that fits around your limb and keeps it tight without causing pain or restricting blood flow in your limb. Whenever the pain flares up, pull the compression sleeve over your limb and keep your arm elevated if you can to keep the fluids from building up. You can use compression socks if your swelling is mainly a problem on your foot or ankle. If you’re in a pinch, you can wrap the limb in a cloth bandage and pin it in place to provide some relief.

Do a self-massage to help with manual lymphatic drainage. You may be able to help your lymphatic system drain by massaging the area around your lymph nodes. Start at your neck and make slow strokes down toward your trunk. Then, make long, slow strokes on your abdomen moving up toward your trunk. Repeat for your groin, back, and sides. Finally, massage your arms, underarms, and legs, making long strokes toward your trunk. The massage shouldn't be painful, so stop if you feel any pain.

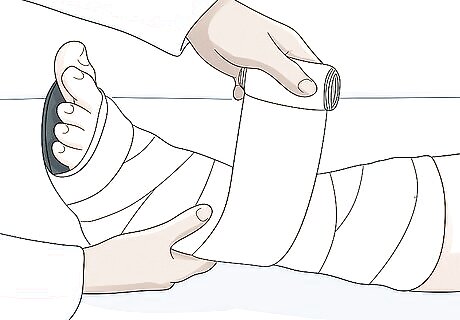
Apply multi-layer bandages as advised by a healthcare professional. You may be able to help your lymphatic system drain by tightly bandaging the area around your lymphedema. Cover the area with padding before you bandage it. Start applying the bandages on the side of your lymphedema that's opposite from your trunk. Then, layer the bandages as you work your way toward the other side of the lymphedema. This will push the fluid toward your trunk. For instance, let's say you had a lymphedema in your arm. You'd cover the arm with cotton or foam to pad it, then start applying the bandage at your hand. Layer the bandages up to your arm pit.
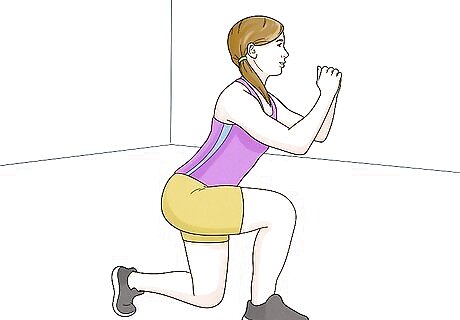
Perform strength-training exercises as directed by your doctor. Strength training may help your lymphatic system work better, especially if you combine it with compression garments. Talk to your doctor to find out what exercises are right for you and ask if you should wear compression garments during your exercises to help with your lymphedema. Follow your doctor's instructions exactly. Your doctor may give you a set of exercises to do.
Complete CDT with a physical therapist to learn how to manage the symptoms. On average, complete decongestive therapy (CDT) will reduce swelling in your lower limbs by 59% and in your upper limbs by 67%. This is a therapeutic treatment you complete with a physical therapist. It involves a combination of compression, drainage, and exercise. You complete the CDT treatment regularly until you develop a routine that reduces your symptoms. This is considered the best way to treat CDT. You’ll need a physical therapist to perform this treatment at first, but they’ll teach you how to do all of this yourself once you find a maintenance plan. Other treatment options include surgery to remove the excess fluid and manual lymph drainage, which is basically a special massage designed to push the fluids out and relieve symptoms.


















Comments
0 comment