
views
Recognizing Symptoms of a Blood Clot

Watch for swelling, especially in an arm or leg. Since clots block your blood flow, blood builds up behind the clot. This excess blood will cause swelling in the area around the clot. Swelling is often the first symptom that you will notice. If your arm or leg is swelling but you haven’t injured yourself, then you may have a blood clot. In some cases, swelling can be severe in size. Pain, tenderness, redness, and warmth in your lower leg could also be a sign of a blood clot.

Notice if you have pain in your shoulder, arm, back, or jaw. Blood clots can cause pain in the location of the clot, or, as in the case of heart attacks, which are caused by blood clots, displaced pain. The pain may feel like a cramp or charley horse. Unlike with a cramp, you will also experience other symptoms such as swelling and discoloration. Any blood clot can cause this type of pain, but it’s especially common with DVT. The pain will be severe and not relieved by over-the-counter pain killers.
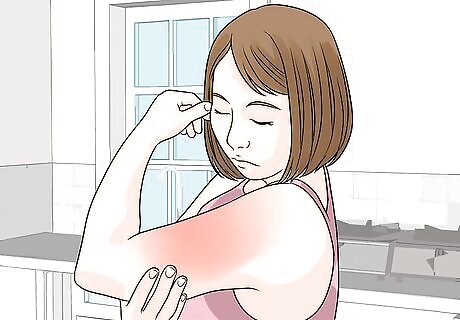
Look for patches of discolored skin. The skin around the swollen area may also have a reddish or bluish discoloration that looks like a bruise that won’t go away. If discolored skin is coupled with swelling and pain, then you should seek immediate medical attention.

Feel to see if your skin is warm. Blood clots cause your skin to be warm to the touch. Place your palm against your skin to feel the temperature. Compare it to the temperature of your forehead to determine if the skin over the potential clot feels warmer. While the warmth may radiate just from the swollen part of your body, your entire limb could be warm. In some cases, your skin may feel hot to the touch, rather than just warm.

Watch for sudden weakness or numbness in your arm, leg, or face. This symptom can be caused by all types of blood clots, including DVT, heart attacks, strokes, and pulmonary embolisms. You may not be able to lift your arm, walk, or speak. If you experience this symptom, you should seek medical care immediately. At first, you may feel clumsy or like your legs are heavy. You may have difficulty speaking or lifting your arms.
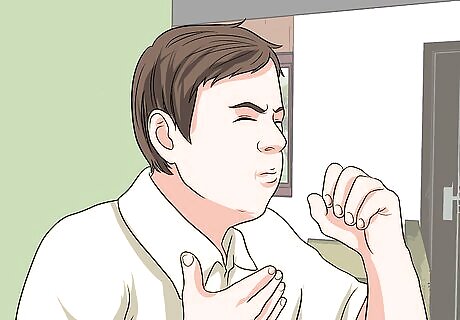
Recognize symptoms of a blood clot in your lungs. A blood clot in your lungs is called a pulmonary embolism. While they share many of the symptoms of blood clots in other parts of your body, they also include a few specific symptoms involving your lungs. Blood clots in the lungs usually have a sudden onset, so you may feel okay but then have symptoms. If you have any of these symptoms, you should call emergency services immediately: A bloody cough. Lightheadedness. Excessive sweating. Chest pain or tightness. Shortness of breath, or painful breathing. Rapid or irregular heartbeat.

Identify a stroke with F.A.S.T. Blood clots are the most common cause of strokes. They often cause headaches, dizziness, trouble seeing, lightheadedness, and trouble walking. Since it’s important to get treatment quickly, you can use the acronym F.A.S.T. to easily identify a stroke. Face- Look for one side of the face drooping. Arms - Check if the person can raise their arms and keep them up. Speech - Is the person’s speech slurred or strange? Time - If you notice any symptoms, act quickly and call emergency services.
Know if you have risk factors. You’re more likely to develop a blood clot if you have risk factors for one. Knowing your risk factors could help you and your doctor determine if your symptoms could be a blood clot. This is particularly important in the early stages when your symptoms may not be that serious. Common risk factors include: Recent hospitalization or a recent orthopedic cast on a lower extremity. Major surgery within 4 weeks Obesity, pregnancy, smoking, surgery, and prior history of stroke. Prolonged sitting or rest, bedrest for more than 3 days. History of pulmonary embolism, DVT, and heart failure. Swelling your entire leg or greater than 3 in (7.6 cm) on your calf. Hiatal hernia, peripheral artery disease, polycythemia vera, and heart arrhythmias. Non-varicose superficial veins. Active cancer or cancer treatment within the past 6 months. Factor V Leiden, family history of blood clots, arteriosclerosis/atherosclerosis, and antiphospholipid syndrome. Certain medications, such as oral contraceptives, hormone therapy, and some breast cancer medications.
Getting a Medical Diagnosis

Consult your doctor immediately if you are experiencing symptoms. Make an appointment with your doctor as soon as possible. Provide your doctor with a list of your symptoms, as well as your risk factors for blood clots. Your doctor will want to examine you and perform diagnostic tests to confirm if you have a blood clot. If you have serious symptoms such as extreme pain, swelling, or weakness, or trouble breathing, you should call emergency services immediately.

Get an ultrasound to check for clots. Your doctor will place the ultrasound wand over the area where a blood clot is suspected. The sound waves from the wand will travel through your body and may provide an image of the clot. Your doctor may do several ultrasounds over a few days to see if the clot is growing. CT or MRI scans can also provide an image of the clot. The most common area for a DVT is your calves, so get any pain in that area evaluated immediately.
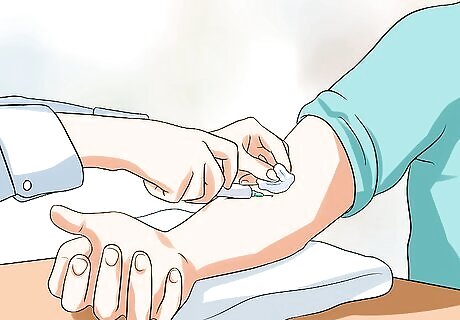
Undergo a blood test to find out if you have high levels of D dimer. D dimer is a protein that can be left in your blood after you've had a blood clot. High levels of D dimer mean that you likely have a blood clot or one that's recently dissolved. Based on the results of your D dimer blood test, your doctor can determine if the symptoms you're experiencing are caused by a blood clot.

Consent to a venography test. Your doctor will inject a contrast solution into your veins, which will mix with your blood and highlight any clots. Your doctor will then take X-rays of the area where the suspected clot is located.
Treating a Blood Clot
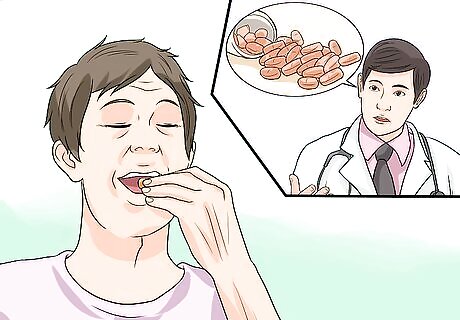
Take anticoagulants as prescribed by your doctor. Once your doctor has diagnosed a blood clot, you will likely be prescribed anticoagulants, such as low-molecular-weight-heparin, which are also called blood thinners. This medication prevents your blood from thickening, which reduces the likelihood that it will form another clot that would cause the vein blockage to worsen. It won’t fix an existing clot, but it will keep the clot from expanding and prevent others from forming. Blood thinners are prescribed based on how long it takes your blood to clot. This is called your prothrombin time (PT) baseline. Your doctor will conduct tests to determine your PT before prescribing blood thinners. Blood thinners can be given as an injection once or twice daily or in pill form. If you’re on blood thinners, take care to avoid accidents and injuries as your blood will be less able to clot. You will likely need to continue taking the blood thinners after the danger has passed so that another clot doesn’t form. Your doctor will conduct blood tests to determine if the dosage of the blood thinners is correct. They will likely need to adjust the dosage frequently. Depending on what medication you’re prescribed, you may need to monitor your PT and international normalized ratio (INR) as often as your doctor recommends.

Ask your doctor about clot busters. A clot buster is injected into your body via an IV or catheter to break up a serious clot. Since they cause a lot of bleeding, they are only used in extreme cases. This treatment will be administered in an intensive care unit.

Allow your doctor to insert a filter if medication is not an option. If you are unable to take medication to prevent clots, then your doctor can insert a filter in your vena cava. This is a large vein in your abdomen. The filter will stop clots that may form from traveling to your lungs. Your doctor will need to do this in an in-patient hospital setting to ensure there are no complications.
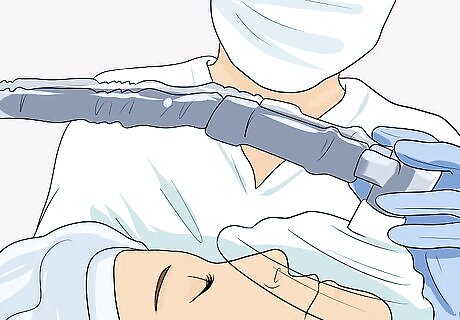
Undergo surgery to remove the clot if other treatments don’t work. Surgery is often the last treatment option for a clot unless you’re in an emergency situation. This surgery is called a thrombectomy. The doctor will open your blood vessel, remove the clot, and then close the vein. They may also install a catheter or a stent to keep the vein open and clot free afterward. Surgery comes with risks and is most often reserved for life-threatening situations.
Preventing Blood Clots

Avoid sitting for long periods. Blood clots are more likely to occur after you’ve been sitting for a long time. Make a point to get up at least every hour during the daytime to walk around for a few minutes. Even if you move slowly or just stand, it’s better than remaining seated all day. Flying on an airplane can be especially risky because you often have to remain seated for a long time. When you fly, get up and walk around the plane, even if it’s just to the bathroom and back. When you must sit for long periods, rotate your ankles and move your legs often. Try to get up and walk around if you can. You can also wear special socks that prevent DVTs while you fly or drive for long periods.

Move around as soon as possible after surgery or bed rest. You should follow all of your doctor’s instructions during your recovery from surgery to prevent blood clots. As soon as recommended, stand and take a short walk around the hospital or care facility. Make sure that you have someone there to help you and offer support so that you don’t fall. It’s normal for you to get up out of bed a day after surgery with supervision.

Wear compression socks or hose to prevent swelling. You should wear them every day to help support your legs and prevent fluid build-up. Socks or stockings should come up to at least your knee. You can buy these at a medical supply shop or get a prescription for them. Getting a prescription can reduce the cost and ensure you get good quality socks. If you’d prefer, you can find hose that covers your whole leg.

Drink at least 8 glasses of water daily. Dehydration increases your risk for blood clots, so make sure you drink enough water. If you don’t like the taste of water, you could drink other beverages like tea or juice.
Lose weight if you are obese. Obesity is a risk factor for blood clots, so losing weight can help you lower your risk. Talk to your doctor before beginning any new diets, exercise programs, or supplements, especially those that claim to help you lose weight. Use a calorie counting app like myfitnesspal to keep up with how much food you're eating and how many calories you're burning. Build your meals around vegetables and lean protein. Limit your intake of added sugars. Increase your activity level after speaking with your doctor. You could try walking, bicycling, dancing, or jogging.

Exercise regularly. Exercise helps you lower your risk of blood clots by helping you maintain your weight and avoid becoming too sedentary. Before you begin any new exercise programs or increase your activity level, you should get approval from your doctor, as increasing activity too quickly can be harmful. Exercise at home by walking, jogging, or bicycling outside or using DVDs. Join a gym for access to a variety of machines and fun group classes. Take a sport like tennis, baseball, or basketball.
Stop smoking. Smoking narrows your veins, making it hard for your blood to flow freely. This increases your risk of blood clots. Quitting can help you lower your risk. You can try quitting on your own or talk to your doctor about using supports for quitting, such as gum, patches, or medications that can help you manage cravings.
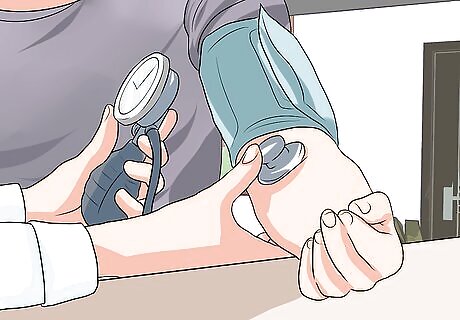
Lower your blood pressure if it’s high. High blood pressure is another risk factor for blood clots that can be managed. If you have high blood pressure, talk to your doctor about creating a treatment plan for lowering it. This may include medications, dietary changes, and exercise. Since high blood pressure is hereditary, you may not be able to lower it back into a normal range without medication, but any progress is helpful.

Lower your cholesterol if it's high. High cholesterol can lead to blood clots because it can lead to fatty deposits that can break off, resulting in a clot. Your doctor can test your blood cholesterol and determine if you are at risk. If your cholesterol is high, you should change your diet accordingly. Your doctor may also prescribe medications to help you manage it.

















Comments
0 comment