
views
Getting your diabetes under control so you can live a happy and healthy life is the goal. The content in this article refers only to general cases and is not intended to replace the opinion of a doctor or following your medical team's advice.
Making a Diabetes Treatment Plan (Type 1 Diabetes)
Consult with a doctor to start or adjust your treatment plan. Type 1 diabetes, also called juvenile diabetes, is a chronic disease, which, despite its name, can begin and affect people at any age. This type of diabetes is an autoimmune disease. While it can occur suddenly due to infection, symptoms will usually appear after an illness. Symptoms in type 1 are usually quite noticeable, more severe and quicker to cause illness. Symptoms for type 1 or advanced type 2 often include: Increased thirst and frequent urination Dehydration Possibly extreme hunger with confused appetite (nothing satisfies you) Unexplained blurred vision Unexplained weight loss Unusual weakness/fatigue Irritability Slow-healing sores Frequent infections (such as gums or skin infections and vaginal infections), Nausea and/or vomiting Ketones in the urine, in medical tests -- ketones are a byproduct of the unhealthy breakdown/loss of muscle and fat (wasting away) that happens when there's not enough available insulin to support life.

Seek medical attention immediately if faced with any of the following severe problems in untreated type 1 or 2 diabetes. These can be life-threatening. They may include: Weakened immunity to infectious diseases Poor circulation (including in the eyes and kidneys) Illnesses, infectious diseases Numbness, tingling in toes and feet Infections slow to heal (if at all) especially in toes and feet Gangrene (dead flesh) in toes, feet, and legs (usually without pain)
Watch for initial symptoms of Type 1 diabetes being severe, it is not uncommon for you to have to stay in the hospital for a short time after your diagnosis. If you suspect that you have diabetes and delay seeing a doctor, you can end up in a coma. Always rely on the advice of a qualified doctor or specialist when deciding on any plans to fight your diabetes. Neither Type 1 nor Type 2 diabetes can be completely cured, but with a lifelong commitment to your treatment plan, these diseases can be managed to the point that you will be able to live a normal life. Begin your treatment plan immediately after you develop diabetes, for better health. If you think you may have diabetes, do not wait on seeing a doctor. It is highly recommended that you see a doctor.

Take steps to understand diabetes. You're here, so you are in the right mindset. Diabetes educators are highly recommended. These experts help you understand the different tools available to you, and can help you adjust your meals to better control blood glucose levels. For those who are diagnosed with type 1 diabetes at a young age, an appointment with a diabetes trainer/educator is often mandatory, and they will often meet with you while in the hospital.

Take your medications every day. The body of a person with Type 1 diabetes needs insulin because their pancreas is damaged in a way that will not produce enough insulin as needed. Insulin is a chemical compound used to break down sugar (glucose) in the bloodstream. Those with type 1 diabetes must work with their doctor to find their correct dosage of insulin, because different individuals have different reactions to various types of insulin, and because some individuals with this type of diabetes may still be producing insulin at mild levels. Without insulin, the symptoms of Type 1 diabetes will rapidly worsen and eventually cause death. To be clear: Individuals with Type 1 diabetes need to take insulin every day or they will die. Your precise daily insulin dosages will vary based on your size, diet, activity level, and genetics, which is why it is so important to see a doctor to get a thorough evaluation before beginning your diabetes treatment plan. Insulin is generally available in several different varieties, each of which is formulated for specific purposes. These are: Rapid-acting: "Mealtime" (bolus) insulin. Usually taken right before a meal to prevent elevated blood glucose levels after eating. Short-acting: Basal insulin. Usually taken between meals once or twice a day to control "resting" blood glucose levels. Long-acting: A combination of bolus and basal insulin. Can be taken before breakfast and dinner in order to keep blood glucose levels low after meals as well as throughout the day. Intermediate-acting: Combined with rapid-acting insulin. It covers the blood glucose elevations when rapid-acting insulins stop working. This type is typically taken twice a day.
Consider an insulin pump. An insulin pump is a device that continually injects a bolus rate insulin to mimic the effects of the basal rate insulin. Your blood glucose level is entered into the device at meal times and in accordance with your normal testing schedule, and your bolus is calculated for you. In addition a carbohydrate ratio can be set and be added to the bolus calculation as well. There is the new tubeless (no tubing) insulin pump that is an "all-in-one" unit that typically come loaded with a three-day supply of insulin with the battery and pump built-in, it is the Omnipod, that is wirelessly controlled by a Personal Diabetes Manager (PDM). It takes ideally about ten pumps per month that come in a box holding a 30-day supply. The old, standard injection set consisted of a plastic cap attached to a catheter that injects the insulin (subcutaneous delivery of insulin). It was inserted into your chosen injection site brought from the pump by tubing called the cannula. The pump set might be attached to a belt or near the delivery site with an adhesive pad. On the other end, the tubing connects to a cartridge that you fill with insulin and insert into the pump unit. Some pumps have a compatible glucose monitor that measures glucose levels just below the dermis. While not as effective as a glucose meter, this device will allow early detection and compensation for sugar spikes and drops. Pump users typically monitor their blood sugars more frequently to evaluate the effectiveness of insulin delivery by the pump, to be aware if the pump malfunctions. Some malfunctions of the insulin pump include: Pump battery is discharged Insulin is inactivated by heat exposure Insulin reservoir runs empty Tubing loosens and insulin leaks rather than being injected The cannula becomes bent or kinked, preventing delivery of insulin.
Exercise. In general, people with diabetes should strive to be physically fit. Physical exercise has the effect of lowering the body's glucose levels - sometimes for as long as 24 hours. Because the most harmful effects of diabetes are caused by elevated glucose levels (blood sugar "spikes"), exercise after eating is a valuable tool that uses sugar naturally and allows people with diabetes to keep glucose at manageable levels. In addition, exercise also provides the same benefits to those with diabetes that it does to those without it - namely, greater overall fitness, weight loss (but rapid weight loss is a bad symptom indicating food and sugar is not used properly by your system). You can gain higher strength and endurance, higher energy levels, elevated mood, and more benefits of exercise as well. Diabetes resources generally recommend exercising at least several times per week. Most resources recommend a healthy mix of cardio, strength training, and balance/flexibility exercises. See How to Exercise for more information. Though low, manageable glucose levels are generally a good thing for moderate activity for people who have diabetes. Exercising vigorously while you have low blood sugar levels can lead to a condition called hypoglycemia, in which the body doesn't have enough blood sugar to fuel its vital processes and the exercising muscles. Hypoglycemia can lead to dizziness, weakness, and fainting. To counter hypoglycemia, carry a sugary, quick-acting carbohydrate with you while you exercise, such as a sweet, ripe orange, or a soda, a sports drink or such as recommended by your health team.
Minimize stress. Whether the cause is physical or mental, stress is known to cause blood sugar levels to fluctuate. Constant or prolonged stress can cause blood sugar levels to rise in the long term, which means you may need to use more medication or exercise more frequently to stay healthy. Generally, the best cure for stress is a preventative one - avoid stress in the first place by exercising frequently, getting enough sleep, avoiding stressful situations when possible, and talking about your problems before they become serious. Other stress management techniques include seeing a therapist, practicing meditation techniques, eliminating caffeine from your diet, and pursuing healthy hobbies. See How to Deal With Stress for more information.
Avoid getting sick. As both an actual physical ailment and as an indirect source of stress, illness can cause your blood sugars to fluctuate. Prolonged or serious illness can even necessitate changes in the way you take your diabetes medication or the diet and exercise routines you'll need to keep. Though the best policy when it comes to illnesses, is to avoid them by living a life that is as healthy, happy, and stress-free as possible. If and when you do come down with an illness, be sure to give yourself the rest and medicine that you need to get better as quickly as possible. If you have the common cold, try drinking plenty of fluids, taking over-the-counter cold medications (but avoid sugary cough syrups), and getting plenty of rest. Since having the cold can ruin your appetite, you'll want to be sure to eat roughly 15 grams of carbohydrates every hour or so. Though having a cold usually elevates your blood sugar levels, refraining from eating as may feel natural can cause your blood sugar to fall dangerously low. Serious illnesses always require the advice of a doctor, but managing serious diseases in patients with diabetes can require special medicines and techniques. If you are a person with diabetes and you think you may have a disease that is more serious than an ordinary cold, see your doctor right away.
Modify your diabetes plans to account for menstruation and menopause. Women with diabetes have unique challenges when it comes to managing blood sugar during their periods and menopause. Though diabetes affects every woman differently, many women report having elevated blood sugar levels in the days before their periods, which can require using more insulin or changing your diet and exercise habits to compensate. However, your blood sugar levels during your menstrual cycle may be different, so talk to your doctor or gynecologist for specific guidance. Additionally, menopause can change the way that the body's blood sugar level fluctuates. Many women report that their glucose levels become more unpredictable during menopause. Menopause can also lead to weight gain, sleep loss, and temporary vaginal ailments, which can increase the body's levels of stress hormones and elevate glucose levels. If you have diabetes and are going through menopause, talk to your doctor to find a treatment plan that's right for you.

Schedule regular check-ups with your doctor. Right after you are diagnosed with Type 1 diabetes, it is likely that you will need to meet with your doctor regularly (as much as once a week or more) to get a sense for how to best control your blood glucose levels. It can take a few weeks to develop an insulin therapy regimen that perfectly matches your diet and activity level. Once your diabetes treatment routine is established, you won't need to meet with your doctor quite as often. However, you should plan on maintaining a good relationship with your doctor, which means scheduling semi-regular follow-up appointments. Your doctor is the person who is best-suited to detecting anomalies to manage your diabetes during times of stress, sickness, pregnancy, and so on. Those with Type 1 diabetes should expect to see their doctor once every 3 - 6 months once a routine is established.
Making a Diabetes Treatment Plan (Type 2 Diabetes)

Consult with your doctor before beginning treatment. If you have Type 2 diabetes, your body is able to produce some insulin, as opposed to none at all, but has a diminished capacity for producing insulin or is not able to use the chemical correctly. Because of this crucial difference, Type 2 diabetes symptoms can be more mild than Type 1 symptoms, and have a more gradual onset, and can require less drastic treatments (though exceptions are possible). However, as with Type 1 diabetes, seeing your doctor before beginning any treatment plan is still essential. Only a qualified medical professional has the knowledge definitively diagnose your diabetes and design a treatment plan that's tailored to your personal needs.
If you can, manage your diabetes with diet and exercise. As noted above, people with Type 2 diabetes have a diminished (but not nonexistent) capacity to make and use insulin naturally. Because their bodies do make some insulin, in some cases, it's possible for people with Type 2 diabetes to manage their disease without having to use any artificial insulin. Usually, this is done through careful diet and exercise, which means minimizing the amount of sugary foods consumed, maintaining a healthy weight, and exercising regularly. Some people with mild cases of Type 2 diabetes can potentially live basically "normal" lives if they are very careful about what they eat and how much they exercise. It's important to remember, however, that some cases of Type 2 diabetes are more severe than others and can't be managed with diet and exercise alone and can require insulin or other medications. Note: see the sections below for information relating to diet and medications.

Be prepared to pursue more aggressive treatment options over time. Type 2 diabetes is known to be a progressive disease. This means that it can get worse over time. This is thought to be because the body's cells responsible for producing insulin get "worn out" from having to work extra hard in people with Type 2 diabetes. As a result, cases of Type 2 diabetes that once required relatively minor treatment options can eventually require more drastic treatments, including insulin therapy, after several years. This is often not due to any fault on the patient's behalf. As with Type 1 diabetes, you should keep in close contact with your physician if you have Type 2 diabetes - regular tests and checkups can help you detect the progression of Type 2 diabetes before it becomes serious.
Consider bariatric surgery if you are obese. Obesity is one of the leading causes of Type 2 diabetes. However, being obese can make any case of diabetes more dangerous and harder to manage. The added stress that obesity puts on the body can make it extremely difficult to keep blood sugar at healthy levels. In Type 2 diabetes cases where patients have high body mass indexes (usually greater than 35), doctors will sometimes recommend weight-reduction surgeries to bring the patient's weight under control quickly. Two types of surgery are usually used for this purpose: Gastric bypass surgery - the stomach is shrunk to the size of a thumb and the small intestine is shortened so that fewer calories are absorbed from food. This change is permanent. Laparoscopic Gastric Banding ("Lap Banding") - a band is wrapped around the stomach so that it feels fuller with less food. This band can be adjusted or removed if needed.
Receiving Diabetes Tests
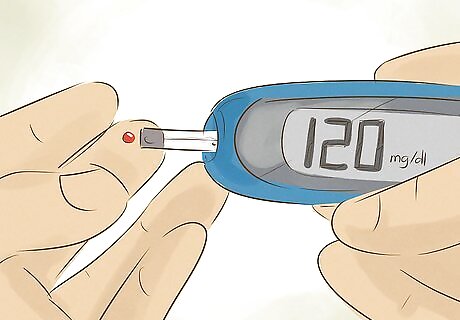
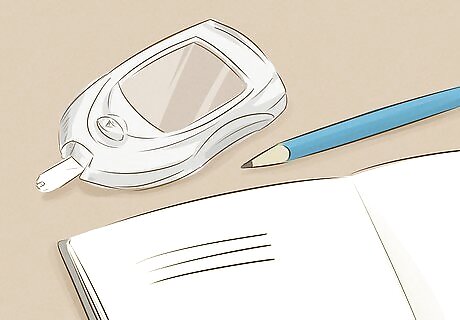
Check your blood sugar every day. Because the potentially harmful effects of diabetes are triggered by elevated blood sugar levels, it's important for people with diabetes to check their blood sugar levels fairly regularly. Today, this is usually done with a small, portable machine that measures your blood sugar from a tiny drop of your blood. The exact answers to when, where, and how you should check your blood sugar can depend on your age, the type of diabetes you have, and your condition. Thus, you'll want to talk to your doctor before beginning to monitor your blood sugar levels. The advice below is for general cases and is not meant to replace the advice of a doctor. Those with Type 1 diabetes are often instructed to check their blood sugar three or more times a day. This is often done before or after certain meals, before or after exercise, before bed, and even during the night. If you are sick or are taking a new medication, you may need to monitor your blood sugar even more closely. Those with Type 2 diabetes, on the other hand, usually don't have to check their blood sugar quite as often - they may be instructed to check their levels once or more per day. In cases where Type 2 diabetes can be managed with non-insulin medications or diet and exercise alone, your doctor may not even require you to check your blood sugar every day.
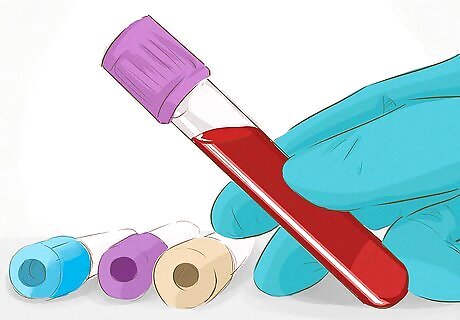
Take an A1C test several times per year. Just as it is important for people with diabetes to monitor their blood sugar from day to day, it's also important to have a "bird's eye" perspective of long-term trends in blood sugar levels. People with diabetes should generally have special test called A1C (also known as Hemoglobin A1C or HbA1C) tests at regular intervals - your doctor may direct you to have such tests every month or every two to three months. These tests monitor the average blood sugar level over the last few months rather than giving an instantaneous "snapshot" and thus can provide valuable information about whether or not a treatment plan is working well. A1C tests work by analyzing a molecule in your blood called hemoglobin. When glucose enters your blood, some of it binds to these hemoglobin molecules. Because hemoglobin molecules usually live for about 3 months, analyzing the percentage of hemoglobin molecules that are bound to glucose can paint a picture of how high blood sugar levels were over the past few months.

Test for ketones in your urine if you have ketoacidosis symptoms. If your body lacks insulin and can't break down the glucose in the blood, its organs and tissues will quickly become starved for energy. This can lead to a dangerous condition called ketoacidosis in which the body begins to break down its fat stores to fuel its important processes. Though this will keep your body functioning, this process produces toxic compounds called ketones which, if allowed to build up, can be potentially life-threatening. If you have a blood sugar reading over 240 mg/dL or exhibit the symptoms listed below, test for ketoacidosis every 4-6 hours (this can be done with a simple over-the-counter urine strip test).If your test reveals you have a high amount of ketones in your urine, call your doctor immediately and seek emergency treatment. The symptoms of ketoacidosis are: Nausea Vomiting Sweet-smelling, "fruity" breath odor Unexplained weight loss.
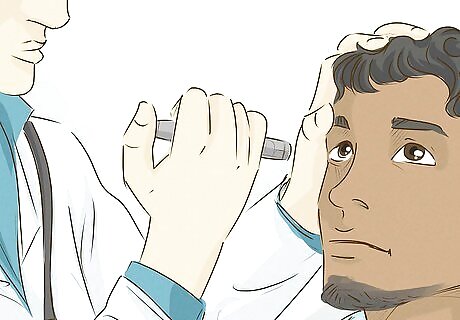
Receive foot and eye tests regularly. Because Type 2 diabetes can progress so gradually that it's difficult to detect, it's important to be on the lookout for possible complications from the disease so that they can be addressed before becoming serious. Diabetes can cause nerve damage and change circulation to certain parts of the body, especially the feet and eyes. Over time, this can result in loss of the feet or blindness. People with Type 1 and people with Type 2 diabetes are both at risk for these complications. However, because Type 2 diabetes can progress gradually without being noticed, it's extra-important to schedule regular foot and eye exams to prevent either condition from developing. Comprehensive dilated eye exams check for diabetic retinopathy (vision loss from diabetes) and should normally be scheduled about once a year. During pregnancy or illness, more-frequent is likely to be necessary. Foot tests check for pulse, feeling, and the presence of any sores or ulcers on the feet and should be scheduled about once per year. However, if you have had foot ulcers before, having tests as often as once every 3 months may be necessary.
Managing Your Diet
Always defer to your dietitian's advice. When it comes to controlling your diabetes, diet is crucial. Carefully managing the types and amounts of foods you eat allows you to manage your blood sugar level, which has a direct effect on the severity of your diabetes. The advice in this section comes from reputable diabetes resources, but every diabetes plan should be individually-tailored for you based on your age, size, activity level, condition, and genetics. Thus, the advice in this section is intended only as a general advice and should never replace the advice of a qualified doctor or nutritionist. If you are unsure of how to obtain personalized diet information, talk to your doctor or general practitioner. S/he will be able to guide your diet plan or refer you to a qualified specialist.
Aim for a low-calorie, high nutrient diet. When someone eats more calories than s/he burns, the body responds by creating an increase in blood sugar. Since the symptoms of diabetes are caused by elevated blood sugar levels, this is undesirable for people suffering from diabetes. Thus, people with diabetes are generally encouraged to eat diets which provide as many essential nutrients as possible while keeping the total calories consumed per day at a sufficiently low level. Thus, foods (like many types of vegetables) which are nutrient-dense and low-calorie can make up a good portion of a healthy diabetes diet. Low-calorie, high-nutrient diets are also helpful for diabetes because they ensure you remain at a healthy weight. Obesity is known to strongly contribute to the development of type 2 Diabetes.Manage Diabetes Risk with Diet and Exercise Step 3.jpg

Prioritize healthy carbohydrates like whole grains. In recent years, a lot of the health dangers posed by carbohydrates have been brought to light. Most diabetes resources recommend eating controlled amounts of carbohydrates - specifically, healthy and nutritious varieties of carbohydrates. Generally, individuals with diabetes will want to limit their intake of carbohydrates to moderately low levels and to make sure that the carbohydrates they do eat are whole grain, high-fiber carbohydrates. See below for more information: Many carbohydrates are grain products, which are derived from wheat, oat, rice, barley, and similar grains. Grain products can be divided into two categories - whole grains and refined grains. Whole grains contain the entire grain, including the nutrient-rich outer portions (called the bran and germ), while refined grains only contain the innermost starchy portion (called the endosperm), which is less nutrient-rich. For a given calorie amount, whole grains are much more nutrient-rich than refined grains, so try to prioritize whole grain products over "white" breads, pastas, rice, and so on. Bread has been shown to raise a person's blood sugar more than two tablespoons of table sugar.
Eat fiber-rich foods. Fiber is a nutrient contained in vegetables, fruits, and other plant-derived foods. Fiber is largely indigestible - when it's eaten, most fiber passes through the intestine without being digested. Though fiber doesn't provide much nutrition, it does provide a variety of health benefits. For instance, it helps control feelings of hunger, making it easier to eat healthy amounts of food. It also contributes to digestive health and is famously known to help "keep you regular". High-fiber foods are a great choice for people with diabetes because they make it easier to eat a healthy amount of food each day. High-fiber foods include most fruits (especially raspberries, pears, and apples), whole grains, bran, legumes (especially beans and lentils), vegetables (especially artichokes, broccoli, and green beans).
Eat lean sources of protein. Protein is often (rightly) lauded as a healthy source of energy and muscle-building nutrition, but some sources of protein can come loaded with fat. For a smarter option, choose low-fat, high-nutrient lean protein sources. In addition to supplying the nutrition needed for a strong, healthy body, protein is also known to produce a greater, longer-lasting feeling of fullness than other sources of calories. Lean proteins include skinless white meat chicken (dark meat has a little more fat, while the skin is high-fat), most fish, dairy products (full-fat is better than low-fat or fat free), beans, eggs, pork tenderloin, and lean varieties of red meat.

Eat some "good" fats, but enjoy these sparingly. Contrary to popular belief, dietary fat isn't always a bad thing. In fact, certain types of fat, namely mono and polyunsaturated fats (which include Omega 3's) are known to provide health benefits, including lowering the body's level of LDL, or "bad" cholesterol. However, all fats are calorie-dense, so you'll want to enjoy fats sparingly to maintain a healthy weight. Try to add small servings of "good" fats into your diet without increasing your overall calorie load per day - your doctor or dietician will be able to help you here. Foods that are rich in "good" fats (mono and polyunsaturated fats) include avocados, most nuts (including almonds, pecans, cashews, and peanuts), fish, tofu, flaxseed, and more. On the other hand, foods that are rich in "bad" fats (saturated and trans fats) include fatty meats (including regular beef or ground beef, bacon, sausage, etc.), fatty dairy products (including cream, ice cream, full-fat milk, cheese, butter, etc.), chocolate, lard, coconut oil, poultry skins, processed snack foods, and fried foods.

Avoid foods rich in cholesterol. Cholesterol is a lipid - a type of fat molecule - that is naturally produced by the body in order to serve as an important part of cell membranes. Though the body naturally requires a certain amount of cholesterol, elevated levels of blood cholesterol can lead to health problems - especially for people with diabetes. High cholesterol levels can lead to a variety of serious cardiovascular problems, including heart disease and stroke. People with diabetes are naturally predisposed to having cholesterol levels that are unhealthy, so it's extra important for diabetes sufferers to monitor their cholesterol intake than for people without the disease. This means choosing foods carefully to limit the intake of cholesterol. Cholesterol comes in two forms - LDL (r "bad") cholesterol and HDL (or "good") cholesterol. Bad cholesterol can build up on the inner walls of the arteries, causing eventual problems heart attack and stroke, while good cholesterol helps remove damaging cholesterol from the blood. Thus, people with diabetes will want to keep their level of "bad" cholesterol intake as low as possible while eating healthy amounts of "good" cholesterol. "Bad" cholesterol sources include: Fatty dairy products, egg yolks, liver and other types of organ meat, fatty meats, and poultry skin. "Good" cholesterol sources include: Oatmeal, nuts, most fish, olive oil, and foods with plant sterols
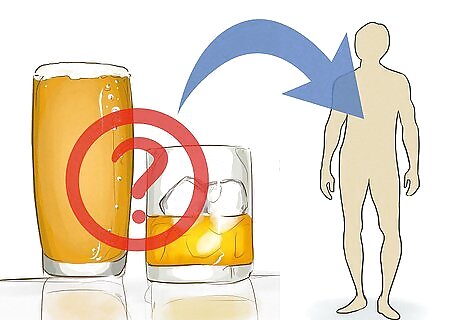
Consume alcohol cautiously. Alcohol is often called a source of "empty calories", and for good reason - alcoholic beverages like beer, wine, and liquor contain calories but little in the way of actual nutrition. Luckily, most people with diabetes can still enjoy these entertaining (if not nutritious) drinks in moderation. According to the American Diabetes Association, moderate alcohol use actually has little effect on blood glucose control and does not contribute to heart disease. Thus, people with diabetes are generally encouraged to follow the same guidelines as people without diabetes when it comes alcohol: men can enjoy up to 2 drinks daily, while women can have 1 drink. Note that, for medical purposes, "drinks" are defined as standard-size servings of the beverage in question - about 12 ounces of beer, 5 ounces of wine, or 1 & 1/2 ounces of liquor. Note also that these guidelines do not account for sugary mixers and additives which may be added to cocktails and can negatively impact the blood glucose level of someone with diabetes.

Use intelligent portion control. One of the most frustrating things about any diet, including a diabetes diet, is that eating too much of any food - even healthy, nutritious food - can cause weight gain which leads to health problems. Because it's important for people with diabetes to keep their weight at a healthy level, portion control is a serious concern. Generally, for a large meal, like dinner, those with diabetes will want to eat plenty of nutritious, fiber-rich vegetables along with controlled amounts of lean protein and starchy grains or carbohydrates. Many diabetes resources offer sample meal guides to help teach the importance of portion control. Most of such guides offer advice that strongly resemble the following: Devote 1/2 of your plate to non-starchy, fiber-rich vegetables like kale, spinach, broccoli, green beans, bok choy, onion, pepper, turnip, tomatoes, cauliflower, and many more. Devote 1/4 of your plate to healthy starches and grains like whole grain breads, oatmeal, rice, pasta, potatoes, beans, peas, grits, squash, and popcorn. Devote 1/4 of your plate to lean protein like skinless chicken or turkey, fish, seafood, lean beef or pork, tofu, and eggs.
Using Medication

Talk to your doctor before taking any medication for your diabetes. Diabetes is a serious illness which can require special medications to treat. However, if misused, these medications can lead to problems which can be serious in their own right. Before taking any medication for your diabetes, talk to your doctor to develop a plan that takes all treatment options (including diet and exercise) into account. Like all serious medical conditions, a case of diabetes requires the advice of a qualified professional. The information in this section is purely informative and should not be used to pick medications or formulate dosages. Additionally, you won't necessarily want to stop taking any medications you are currently on if you discover you are have diabetes. A doctor must evaluate all of the variables at play - including your current medication usage - to develop a plan to treat your diabetes. The effects of using too much or too little diabetes medication can be serious. For instance, an overdose of insulin can result in hypoglycemia, leading to dizziness, fatigue, confusion, and even coma in severe cases.
Use insulin to control your blood sugar. Insulin is perhaps the most well-known diabetes medication. The insulin that doctors prescribe to people who have diabetes is a synthetic form of a chemical naturally produced by the pancreas to process sugar in the blood. In healthy individuals, after a meal, when blood sugar levels are high, the body releases insulin to break down the sugar, removing it from the bloodstream and rendering it into a usable form of energy. Administering insulin (via injection) allows the body to process blood sugar properly. Since medicinal insulin comes in several strengths and varieties, it's important to receive a doctor's advice before starting to use insulin. Note that people with Type 1 Diabetes must take insulin. Type 1 diabetes is characterized by the body being completely unable to make insulin, so it must be added by the patient. People with Type 2 Diabetes may or may not take insulin depending upon the severity of their disease.

Use oral diabetes medications to control your blood sugar. There are a variety of options when it comes to orally-administered diabetes medications (pills). Often, for people with moderate cases of Type 2 diabetes, doctors will recommend trying these types of medications before using insulin as the latter represents a more drastic, life-affecting treatment option. Because there are such a wide variety of oral diabetes medications with different mechanisms of action, it's important to talk to a doctor before starting to take any sort of diabetes pills to ensure that the medication is safe for your own personal use. See below for the different types of oral diabetes medications and a brief description of the mechanism of action for each: Sulfonylureas - stimulate the pancreas to release more insulin. Biguanides - lower the amount of glucose produced in the liver and makes muscle tissue more sensitive to insulin. Meglitinides - stimulate the pancreas to release more insulin. Thiazolidinediones - reduce glucose production in liver and increase insulin sensitivity in muscle and fat tissue. DPP-4 inhibitors - prevent the breakdown of normally short-lived chemical mechanisms which regulate the level of blood glucose. SGLT2 Inhibitors - absorbs blood glucose in the kidneys. Alpha-glucosidase inhibitors - lower glucose levels by preventing the breakdown of starches in the intestine. Also slow the breakdown of some sugars. Bile Acid Sequestrants - reduces cholesterol and simultaneously lowers glucose levels. The method for the latter is still not well understood.

Consider supplementing your treatment plan with other medications. The medications specifically designed to fight diabetes above are not the only medications prescribed for diabetes. Doctors prescribe a range of medications, from aspirin to flu shots, to help manage diabetes. However, even though these medications are usually not as "serious" or drastic as the diabetes medications described above, it's usually a good idea to consult with your doctor before supplementing your treatment plan with one of these medicines just in case. Just a few supplementary medicines are listed below: Aspirin - sometimes prescribed to reduce the risk of heart attacks for people with diabetes. Mechanism of action is not well-understood but is thought to relate to aspirin's ability to prevent red blood cells from sticking together. Flu shots - since the flu, like many illnesses, can cause blood glucose levels to fluctuate and make diabetes harder to manage, doctors often recommend that patients receive yearly flu shots to reduce their chance of contracting this disease. Herbal supplements - though most "homeopathic" supplements have not definitively been proven effective in a scientific setting, some diabetes patients offer anecdotal testimonies to their effectiveness.



















Comments
0 comment